Dr. Alo's Cholesterol, Lipids, Diet, Weight Loss, Nutrition, and Fitness Studies!
Most Popular and Cited Studies in My Content!
Sign Up For My Healthy Living Newsletter and Get More Like This in Your Inbox! Join over 200,000 interested in healthy living and cardiology!
Totally FREE!
Don't Worry I Will NEVER Spam You!
Dr. Alo Has Been Featured on Multiple Media Outlets Locally, Nationally, and Internationally!


All The Studies You Need to Battle the Most Common Health, Weight Loss, Nutrition, Cholesterol, and Cardiology Myths Being Perpetrated by Influencers and Social Media Crowd!
This section contains tons more research articles that you can read on this topic broken up into sections. I highly encourage you to read more and study more! Informed consumers are the best and most successful at health, fitness, weight loss, and life in general!
Pathophysiology of Coronary Artery Disease
Good place to start if you want an introduction to coronary artery disease.
https://www.ahajournals.org/doi/full/10.1161/CIRCULATIONAHA.105.537878
Cholesterol, LDL, CVD, and ASCVD
LDL causes ASCVD Ference and Boren EAS:
Ference:
https://academic.oup.com/eurheartj/article/38/32/2459/3745109
Boren:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7308544/
Treat ASCVD Earlier and Stronger: (Peter Toth)
Atherosclerotic cardiovascular disease (ASCVD) is epidemic throughout the world and is etiologic for such acute cardiovascular events as myocardial infarction, ischemic stroke, unstable angina, and death. ASCVD also impacts risk for dementia, chronic kidney disease peripheral arterial disease and mobility, impaired sexual response, and a host of other visceral impairments that adversely impact the quality and rate of progression of aging. The relationship between low-density lipoprotein cholesterol (LDL-C) and risk for ASCVD is one of the most highly established and investigated issues in the entirety of modern medicine. Elevated LDL-C is a necessary condition for atherogenesis induction. Basic scientific investigation, prospective longitudinal cohorts, and randomized clinical trials have all validated this association. Yet despite the enormous number of clinical trials which support the need for reducing the burden of atherogenic lipoprotein in blood, the percentage of high and very high-risk patients who achieve risk stratified LDL-C target reductions is low and has remained low for the last thirty years. Atherosclerosis is a preventable disease. As clinicians, the time has come for us to take primordial and primary prevention more serously. Despite a plethora of therapeutic approaches, the large majority of patients at risk for ASCVD are poorly or inadequately treated, leaving them vulnerable to disease progression, acute cardiovascular events, and poor aging due to loss of function in multiple visceral organs. Herein we discuss the need to greatly intensify efforts to reduce risk, decrease disease burden, and provide more comprehensive and earlier risk assessment to optimally prevent ASCVD and its complications. Evidence is presented to support that treatment should aim for far lower goals in cholesterol management, should take into account many more factors than commonly employed today and should begin significantly earlier in life.
https://www.sciencedirect.com/science/article/pii/S2666667722000551?via%3Dihub
Cholesterol Years
The longer we allow LDL-C to stay elevated, the worse people do. There is no reason to wait until someone is 50+ years old to initiate lipid lowering therapy. It's better to treat it earlier to prevent accumulation of plaque.
From the study:
One of the key clinical insights derived from this analysis is that the long-term risk of a future cardiovascular event is significantly influenced by the level of LDL-C elevation early in life (e.g., age 18 to 30 years) even if LDL-C is lower later in life. These data are concordant with Mendelian randomization studies demonstrating that genetically gifted individuals endowed with low levels of LDL-C from birth demonstrate a disproportionately large benefit on lifelong cardiovascular health. Taken together, these observations suggest that early interventions (primordial and primary prevention) to lower LDL-C may be more effective than later ones. More pragmatically, late interventions to reduce LDL-C fail to eliminate much of the risk accumulated during early exposures. It is clear from randomized controlled trials of intense LDL-C–lowering therapies (e.g., PCSK9 inhibitors) that once a critical mass of atherosclerotic plaque is present, recurrent event rates remain alarmingly high, and this residual risk appears to be only partially and modestly modifiable, at least with intermediate durations of therapy. In the current approach to prevention of atherosclerotic events, we are not using effective tools (e.g., therapeutic lifestyle changes, lipid-lowering therapies, antihypertensive therapies, and so on) to maximum potential.
https://www.jacc.org/doi/10.1016/j.jacc.2020.08.004
Calculating Absolute Risk Reduction from Statins
This study looked at how we can determine absolute risk reduction from statins and how they are actually much higher than reported.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.121.057631
Evaluating the Association Between Low-Density Lipoprotein Cholesterol Reduction and Relative and Absolute Effects of Statin Treatment: A Systematic Review and Meta-analysis
Lowering LDL via statins reduced all cause mortality. For every 1mmol/dl reduction in LDL-C, you reduced all cause mortality by 10%.
https://pubmed.ncbi.nlm.nih.gov/35285850/
Metabolically healthy Young People:
PESA Trial. Preventing Early Subclinical Atherosclerosis
What if we could detect soft plaque before it happens in young people? Long before they are calcified, irreversible plaque?
Only 15% of PESA participants were obese.
PESA Trial (Prevention of Early Subclinical Atherosclerosis) showing that 45% of adults with "normal" LDLs of 100-110 had plaque burden in their arteries (subclinical atherosclerosis). Over 60% of those had it in more than one arterial bed. 58% of people with LDL of 130 had ASCVD and 65% of those with LDL 150 had plaque:
https://www.sciencedirect.com/science/article/pii/S0735109721051159
A meta analysis and meta regression looked at 34 trials and over 130,000 patients and compared intensive versus less intensive lipid lowering therapy. They demonstrated that all-cause mortality and cardiovascular mortality. The effect was more pronounced if their baseline LDL was above 100, and even more pronounced if it was over 160:
https://jamanetwork.com/journals/jama/fullarticle/2678614
From the Article verbatim:
Conclusions and Relevance In these meta-analyses and meta-regressions, more intensive compared with less intensive LDL-C lowering was associated with a greater reduction in risk of total and cardiovascular mortality in trials of patients with higher baseline LDL-C levels. This association was not present when baseline LDL-C level was less than 100 mg/dL, suggesting that the greatest benefit from LDL-C–lowering therapy may occur for patients with higher baseline LDL-C levels.
Another Study on Metabolically Healthy Young People
CARDIA study of 5115 Young Men Starting at Age 18 showed Lowest LDL had negative time to index visit in years. Highest LDL levels had a straight line increasing from 0-10 years with multiple visits for events. Low LDL was below 90, High was over 110 and up to 130.
https://pubmed.ncbi.nlm.nih.gov/34266580/
2019 EAS/ESC Guidelines for the management of dyslipidemias and lipid modification to reduce cardiovascular risk
https://academic.oup.com/eurheartj/article/41/1/111/5556353?login=false
Article in British Medical Journal looking at over 100,000 participants showing that the lower the LDL, the less likely you are to die of heart disease, but may die of cancer (mainly because you live longer). Myocardial infarction was lower in lipid treatment arm with the lowest LDL. All cause mortality, was lower in lipid treatment arm. :
https://www.bmj.com/content/371/bmj.m4266
An article in JAMA looked at whether or not there was benefit in lowering LDL to below 70. They found a 22% relative risk reduction in major adverse cardiovascular events (MACE) for every 1mmol/dL reduction in LDL:
https://jamanetwork.com/journals/jamacardiology/fullarticle/2695047
From the Article:
Conclusions and Relevance There is a consistent relative risk reduction in major vascular events per change in LDL-C in patient populations starting as low as a median of 1.6 mmol/L (63 mg/dL) and achieving levels as low as a median of 0.5 mmol/L (21 mg/dL), with no observed offsetting adverse effects. These data suggest further lowering of LDL-C beyond the lowest current targets would further reduce cardiovascular risk.
An article in the Journal of the American College of Cardiology using Mendelian randomization and meta analysis to evaluate over 300,000 patients and found prolonged exposure to LDL was dangerous and that it needed to be treated earlier in life. They also noted a 54% reduction in cardiovascular disease risk for every 1mmol/dL reduction in LDL if it was started earlier in life. This was three times more effective than waiting and starting a statin later in life:
https://www.sciencedirect.com/science/article/pii/S0735109712047730
Another meta analysis looked at 170,000 patient in 26 randomized trials and also noted reduced cardiovascular disease with more aggressive lowering of LDL. Compared to less intensive therapy, they found that more aggressive lipid lower therapy reduced major cardiovascular events by 15%, reduced myocardial infarctions (heart attacks) by 13%, revascularization (stents, PCI) by 19%, and stroke by 16%, all-cause mortality by 10% for every 1mmol/dL extra reduction in LDL. And none of those deaths from all-cause mortality were excess deaths due to cancer from just living longer:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(10)61350-5/fulltext
Their conclusions:
Further reductions in LDL cholesterol safely produce definite further reductions in the incidence of heart attack, of revascularisation, and of ischaemic stroke, with each 1·0 mmol/L reduction reducing the annual rate of these major vascular events by just over a fifth. There was no evidence of any threshold within the cholesterol range studied, suggesting that reduction of LDL cholesterol by 2–3 mmol/L would reduce risk by about 40–50%.
An article in Circulation looking at over 36,000 patients followed for a median of 26.8 years noted 50-80% increase in relative risk of CVD mortality for those with LDL (and non-HDL) of greater than 160. They also noted that LDL over 190 results in 40% higher CVD mortality.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.034273
Updated 2023 EAS Consensus on Homozygous FH
https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehad197/7148157
Mummies Had ASCVD
https://www.sciencedirect.com/science/article/abs/pii/S0002870319301711
https://www.sciencedirect.com/science/article/abs/pii/S014067361360598X
Conclusions
We found evidence of atherosclerosis in different vascular beds of mummy samples across various time periods and among different cultures, supporting previous findings.7 Noninvasive near-infrared spectroscopy is a promising technique for studying ancient mummies of various cultures to gain insight into the origins of atherosclerosis. Near-infrared spectroscopy has the ability to detect cholesterol-rich atherosclerotic plaques. This noninvasive technique provides further information beyond CT
Atherosclerosis was common in four preindustrial populations including preagricultural hunter-gatherers. Although commonly assumed to be a modern disease, the presence of atherosclerosis in premodern human beings raises the possibility of a more basic predisposition to the disease.
Physiologic LDL in hunter gatherer tribes as low as 50-70 mg/dL
https://pubmed.ncbi.nlm.nih.gov/15172426/
Perhaps even lower:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5937425/
Plaque regression occurs when very low LDL-C levels are achieved in REVERSAL, ASTEROID, SATURN, and GLAGOV trials
https://pubmed.ncbi.nlm.nih.gov/16126025/
https://pubmed.ncbi.nlm.nih.gov/24381872/
https://pubmed.ncbi.nlm.nih.gov/27846344/
https://pubmed.ncbi.nlm.nih.gov/17635739/
https://pubmed.ncbi.nlm.nih.gov/16533939/
https://pubmed.ncbi.nlm.nih.gov/21446892/
Lipid Link True Modifiable Risk Factors
Most influencers online try to claim that diabetes and metabolic syndrome are the true "cause" of athersclerosis. Here are the 9 most modifiable risk factors for a first heart attack: (notice Lipids is first, diabetes is second to last)
https://www.lipidlink.com/CV-event-risk-and-LDL-C.html
Very Low LDL is Safe, as low as 7.7
https://pubmed.ncbi.nlm.nih.gov/28859947/
No Lower Bound for LDL in Secondary Prevention
Ok to get LDL below 55 for secondary prevention.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.123.064041
It's the Cholesterol, Stupid!
An old but good one.
https://www.ajconline.org/article/s0002-9149(10)01954-5/fulltext
Cardiovascular risk in patients achieving low-density lipoprotein cholesterol and particle targets
Conclusions: In this real-world sample of commercially insured patients, higher LDL-P levels were associated with increased CHD risk. Moreover, high-risk patients who achieved LDL-P <1000 nmol/L received more aggressive lipid-lowering therapy than patients achieving LDL-C <100 mg/dL, and these differences in lipids and therapeutic management were associated with a reduction in CHD/stroke events over 12, 24 and 36 months follow-up.
https://pubmed.ncbi.nlm.nih.gov/24956532/
A Long-term Benefit Approach vs Standard Risk-Based Approaches for Statin Eligibility in Primary Prevention
When looking at 30 year, instead of ten year risk assessments, the number needed to treat for statins is 7.
Importance A 10-year benefit-based approach to statin therapy in primary prevention includes younger individuals with higher low-density lipoprotein cholesterol (LDL-C) and prevents more cardiovascular events than a risk-based approach. However, a 10-year treatment duration likely underestimates the expected benefits of statins.
Objective To model the impact of a 30-year benefit approach to select individuals for statin therapy.
Conclusions and Relevance A long-term benefit approach to statin eligibility identifies nearly 1 in 6 individuals as having a high degree of expected long-term benefit of statins, with a number needed to treat of less than 7. This approach identifies younger individuals with higher LDL-C levels who would not be currently recommended for treatment and may provide a more optimal approach for determining statin eligibility in primary prevention.
https://jamanetwork.com/journals/jamacardiology/fullarticle/2706611
Discordance between apolipoprotein B and low-density lipoprotein particle number is associated with insulin resistance in clinical practice
Discordance between ApoB and LDL-C with NMR with insulin resistance.
https://pubmed.ncbi.nlm.nih.gov/25911082/
Meta Analysis of 26 studies showing that All Cause Mortality Lower by Lowering LDL
"Across all 26 trials, all-cause mortality was reduced by 10% per 1·0 mmol/L LDL reduction (RR 0·90, 95% CI 0·87-0·93; p<0·0001)"
https://pubmed.ncbi.nlm.nih.gov/21067804/
Statins reduced all cause mortality by 14% in primary prevention
Conclusions and Relevance In adults at increased CVD risk but without prior CVD events, statin therapy was associated with reduced risk of all-cause and cardiovascular mortality and CVD events, with greater absolute benefits in patients at greater baseline risk.
https://jamanetwork.com/journals/jama/fullarticle/2584057
LIPID Study Showed Pravastatin Reduced CV Mortality and All Cause Mortality in 6 Years
And this with pravastatin, one of the weaker statins.
Original in Lancet:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(02)08351-4/fulltext
“The study showed that taking statins for 6 years reduced death from cardiovascular disease by 24 percent, and overall mortality by 23 percent.”
Statins are associated with a large reduction in all-cause mortality in women from a cardiac outpatient population
"Median follow-up in the matched cohort was 5.8 (3.5–7.9) years, during which 1035 patients (50% women) died. Cardiovascular deaths accounted for a total of 270 events (26% of total). In the whole cohort, statin use reduced the risk of all-cause mortality by 24% (HR 0.76, 95% CI 0.71 to 0.82) and the risk of cardiovascular mortality by 28% (HR 0.72, 95% CI 0.61 to 0.83). This protective effect was stronger in women, with a 34% lower all-cause mortality risk (HR 0.66, 95% CI 0.58 to 0.74) and a 45% lower cardiovascular mortality risk (HR 0.55, 95% CI 0.39 to 0.71) in statin users compared with non-users. A similar but weaker trend was seen for men, with an 11% reduction in all-cause mortality (HR 0.89, 95% CI 0.81 to 0.96) and a non-significant 7% reduction in cardiovascular mortality (HR 0.93, 95% CI 0.77 to 1.08) in statin users compared with non-users. The interaction term for sex was statistically significant for both all-cause mortality (p value for interaction=0.040) and cardiovascular mortality (p value for interaction=0.035)."
https://openheart.bmj.com/content/9/1/e001900
Effect of Statins on All-Cause Mortality in Adults: A Systematic Review and Meta-Analysis of Propensity Score-Matched Studies
"The risk of all-cause mortality was significantly reduced in statin users (hazard ratio: 0.72, 95% confidence interval: 0.66−0.76)."
https://pubmed.ncbi.nlm.nih.gov/36233511/
Adults 50 to 75 Have Significant Benefits from Statin Use for Primary Prevention
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2773065
Statin Side Effects in 9% of People Taking Them, Meta Analysis With Over 4 million
Conclusion: Based on the present analysis of >4 million patients, the prevalence of SI is low when diagnosed according to international definitions. These results support the concept that the prevalence of complete SI might often be overestimated and highlight the need for the careful assessment of patients with potential symptoms related to SI.
https://academic.oup.com/eurheartj/article/43/34/3213/6529098
Transcytosis may play a role, not just passive diffusion of LDL-P
https://www.hindawi.com/journals/omcl/2022/2253478/
Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications
https://pubmed.ncbi.nlm.nih.gov/17938300/
Global look at cholesterol reduction across 5 continents and 88 countries, we need to do better:
https://academic.oup.com/eurheartj/article/44/25/2305/7216561
Insulin resistance is not necessary for ASCVD
Chronic hyperinsulinemia does not increase the production rate of high-density lipoprotein apolipoprotein AI: evidence from a kinetic study in patients with insulinoma
https://pubmed.ncbi.nlm.nih.gov/23908245/
Endogenous chronic hyperinsulinemia does not increase the production rate of VLDL apolipoprotein B: proof from a kinetic study in patients with insulinoma
https://pubmed.ncbi.nlm.nih.gov/21430026/
Absence of clinically overt atherosclerotic vascular disease and adverse changes in cardiovascular risk factors in 70 patients with insulinoma
https://pubmed.ncbi.nlm.nih.gov/8144864/
Treating triglycerides down reduces CV risk.
https://www.atherosclerosis-journal.com/article/S0021-9150(23)05081-5/fulltext
Lipid distributions across the world maps
https://academic.oup.com/eurheartj/article/44/25/2305/7216561
Repatha Showed Plaque changes and regression with images
Conclusions: The combination of statin and evolocumab after a non-ST-segment elevation myocardial infarction produces favorable changes in coronary atherosclerosis consistent with stabilization and regression. This demonstrates a potential mechanism for the improved clinical outcomes observed achieving very low LDL-C levels following an acute coronary syndrome. (Imaging of Coronary Plaques in Participants Treated With Evolocumab). 2022
https://pubmed.ncbi.nlm.nih.gov/35431172/
Effect of Evolocumab on Coronary Plaque Composition
Conclusions: The addition of evolocumab to a statin did not produce differential changes in plaque composition compared with statin monotherapy. This suggests that evaluation of plaque morphology using virtual histology imaging may provide no incremental information about the plaque effects of evolocumab beyond measurement of plaque burden. (GLobal Assessment of Plaque reGression With a PCSK9 antibOdy as Measured by intraVascular Ultrasound [GLAGOV]. 2018
https://pubmed.ncbi.nlm.nih.gov/30336824/
ALL LDL Particles Are Atherogenic, Not Just Small Dense or Oxidized
This is a great article to read that is a great review of atherosclerosis and the role LDL plays in atherogenisis.
https://pubmed.ncbi.nlm.nih.gov/31642874/
Conclusion: The net result is, with the exceptions of the abnormal chylomicron remnants in type III hyperlipoproteinemia and lipoprotein (a), all apoB particles are equally atherogenic.
LDL Particle Size vs Total LDL
Article proving without question, based on meta analysis and Mendelian Genetics that LDL CAUSES heart disease (ASCVD)
High cholesterol and high LDL cause atherosclerotic heart disease. This is based on the consensus statement of the European Atherosclerotic Society Consensus Panel. (https://pubmed.ncbi.nlm.nih.gov/28444290/)
The above article is also another great overall review on cholesterol and atherosclerosis.
The conclusion, verbatim from their published data:
Conclusion: Consistent evidence from numerous and multiple different types of clinical and genetic studies unequivocally establishes that LDL causes ASCVD.
Boren's group re examined the article above a few years later and concluded the same thing:
https://academic.oup.com/eurheartj/article/38/32/2459/3745109
LDL Particle Count Definitely Matters
Articles demonstrating that LDL particle counts matter:
https://pubmed.ncbi.nlm.nih.gov/36111155/
Why Arteries get ASCVD and not Veins?
Articles discussing why arteries get ASCVD and not veins:
Response to Retention:
https://www.ahajournals.org/doi/10.1161/01.ATV.15.5.551
More up to date information in Boren article:
https://academic.oup.com/eurheartj/article/41/24/2313/5735221
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7308544/
Articles concluding that relying on LDL oxidation state are inconclusive and unreliable:
Circulating oxidized LDL was thought to be dangerous and atherogenic. Our immune systems remove oxidized particles very quickly. The amount of circulating oxidized LDL is very minimal. OxLDL lab test simply mad the labs a lot of money and were a meaningless test.
https://pubmed.ncbi.nlm.nih.gov/20816951/
https://pubmed.ncbi.nlm.nih.gov/9470066/
https://pubmed.ncbi.nlm.nih.gov/15467487/
https://pubmed.ncbi.nlm.nih.gov/18091649/
Article summarizing the latest data and research on LDL size and oxidation:
Current Opinion Lipidology Journal Jun 2017:
LDL particle number and size and cardiovascular risk: anything new under the sun?
The authors did an extensive overview of the data on LDL total and size. They concluded:
"LDL particle size, on the other hand, has not been independently associated with CVD risk after adjustment for other risk factors such as LDL cholesterol, triglycerides, and HDL-C and that routine use of information pertaining to particle size to determine and manage patients' risk is not yet justified."
https://pubmed.ncbi.nlm.nih.gov/28460374/
Lowering LDL in Primary and Secondary Prevention
Significant reduction in MACE with lower LDL in primary and secondary prevention. This does not even include all the most recent trials.
https://www.ccjm.org/content/83/3/181
How Low Can You Go? New Evidence Supports No Lower Bound to Low-Density Lipoprotein Cholesterol Level in Secondary Prevention
https://www.ahajournals.org/doi/abs/10.1161/CIRCULATIONAHA.123.064041
All Cause Mortality Should not be the goal when assessing Preventative Medical Therapies
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.116.023359
Conclusion: Evidence-based medicine should not be about withholding interventions until they have been proven to reduce overall mortality. It should be analytic and intelligent, assessing the efficacy and harms of an intervention separately, and then applying these estimates to populations that might be offered the intervention, taking all evidence into account, including an assessment of whether it provides reasonable value for money.
Niacin makes HDL more atherogenic:
https://www.ahajournals.org/doi/10.1161/ATVBAHA.121.316278
6 Supplements Did not Reduce LDL
Cleveland Clinic study showed that very low dose Statin vs garlic, red yeast rice, placebo, fish oil, turmeric, plant sterols:
https://www.jacc.org/doi/10.1016/j.jacc.2022.10.013
Press release:
https://newsroom.clevelandclinic.org/2022/11/06/cleveland-clinic-trial-finds-six-widely-used-dietary-supplements-do-not-lower-cholesterol-compared-with-either-a-low-dose-statin-or-placebo/
Extreme Dietary Cholesterol Intake, can Increase CVD and All Cause Mortality
https://jamanetwork.com/journals/jama/fullarticle/2728487
How much can you lower your cholesterol with diet and exercise
Over 84 studies have been included in a recent meta-analysis and meta-regression which examined the effects of changes in fat type on lipid levels. An absolute 1% reduction in saturated fat or trans fat intake as a percentage of energy with replacement by n-6 polyunsaturated fat would lead to a reduction in low density lipoprotein (LDL) cholesterol of 0.05 mmol/L. In most Western countries the difference in intake between the highest quintile and the lowest quintile of saturated fat is about 7%, so moving from the highest to the lowest quintile should lower LDL cholesterol by 0.35 mmol/L or about 10%. This change should lower cardiovascular disease rates by at least 10%.
https://pubmed.ncbi.nlm.nih.gov/30528924/
When you correct for ApoB, no ratios really matter:
https://www.lipidjournal.com/article/S1933-2874(10)00044-9/fulltext
https://pubmed.ncbi.nlm.nih.gov/21122647/
https://pubmed.ncbi.nlm.nih.gov/23068583/
https://pubmed.ncbi.nlm.nih.gov/15492304/
https://pubmed.ncbi.nlm.nih.gov/14581403/
https://pubmed.ncbi.nlm.nih.gov/19450572/
ApoB better than non-HDL at prediction of ASCVD, risk, events, mortality
https://www.ahajournals.org/doi/10.1161/01.cir.0000145660.60487.94
Using HDL in any Ratio is Inaccurate because, African Americans, Women and other races have different HDL patterns and levels.
https://www.jacc.org/doi/10.1016/j.jacc.2022.09.027
After following 24k participants for 10 years that had never had a prior event.
Conclusions:
Low-density lipoprotein cholesterol and triglycerides modestly predicted CHD risk in Black and White adults. Low HDL-C was associated with increased CHD risk in White but not Black adults, and high HDL-C was not protective in either group. Current high-density lipoprotein cholesterol–based risk calculations could lead to inaccurate risk assessment in Black adults.
Note: High HDL-C was not protective in either group.
BMJ Article Debunking "The Cholesterol Myth Book". The authors were dishonest, made up data, and lied to the public and admitted to all of it.
Genetic Mutations that Confer Genes That Have Genetically Low LDL offer more protection against heart disease and confer longevity
It has long been thought that some members of the people that live in blue zones have genetic mutations that conferred protection against cardiovascular disease due to low or very low LDL, here are the articles on this topic:
https://pubmed.ncbi.nlm.nih.gov/19415983/
https://pubmed.ncbi.nlm.nih.gov/19196970/
https://pubmed.ncbi.nlm.nih.gov/16554528/
https://pubmed.ncbi.nlm.nih.gov/20699424/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2423314/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4087084/
https://www.ahajournals.org/doi/10.1161/01.atv.0000176191.64314.07
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2423314/
PCSK9 Genetic Mutations and Overview
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5976255/
https://www.nature.com/articles/ng1509
The Effects of Carbohydrate versus Fat Restriction on Lipid Profiles in Highly Trained, Recreational Distance Runners: A Randomized, Cross-Over Trial
https://pubmed.ncbi.nlm.nih.gov/35334791/
Role of liver in the maintenance of cholesterol and low density lipoprotein homeostasis in different animal species, including humans
https://pubmed.ncbi.nlm.nih.gov/8245716/
Article Summarizing the Last Four Decades of Lipid Lowering. What has had the most impact? By International Lipid Expert Panel (ILEP)
More Lean Body Mass Increases Longevity:
https://pubmed.ncbi.nlm.nih.gov/37209044/
https://pubmed.ncbi.nlm.nih.gov/24561114/
Low muscle mass increases all-cause mortality:
https://pubmed.ncbi.nlm.nih.gov/37285331/
About 11.3% of population has diabetes, and 90-95% is type 2 (about 9%)
https://www.cdc.gov/diabetes/data/statistics-report/index.html
About 15-40%have insulin resistance
https://bmcendocrdisord.biomedcentral.com/articles/10.1186/s12902-020-00558-9
According to CDC 9.4% of Americans have Type 2 Diabetes, and 29% of women and 36% of men have pre-diabetes
https://www.cdc.gov/media/releases/2017/p0718-diabetes-report.html
Seed Oils Are Cardioprotective
Multiple studies now show that Seed Oils (Linoleic acid, LA, and AA) reduce CVD:
Perhaps the most comprehensive is the first link below. They looked at 68k participants for 31.9 years of follow up and the endpoints were reached 15k times.
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.038908
Results:
In 30 prospective studies with medians of follow-up ranging 2.5 to 31.9 years, 15 198 incident cardiovascular events occurred among 68 659 participants. Higher levels of LA were significantly associated with lower risks of total CVD, cardiovascular mortality, and ischemic stroke, with hazard ratios per interquintile range of 0.93 (95% CI, 0.88–0.99), 0.78 (0.70–0.85), and 0.88 (0.79–0.98), respectively, and nonsignificantly with lower coronary heart disease risk (0.94; 0.88–1.00). Relationships were similar for LA evaluated across quintiles. AA levels were not associated with higher risk of cardiovascular outcomes; in a comparison of extreme quintiles, higher levels were associated with lower risk of total CVD (0.92; 0.86–0.99). No consistent heterogeneity by population subgroups was identified in the observed relationships.
Conclusions:
In pooled global analyses, higher in vivo circulating and tissue levels of LA and possibly AA were associated with lower risk of major cardiovascular events. These results support a favorable role for LA in CVD prevention.
Soybean oil lowers circulating cholesterol levels and coronary heart disease risk, and has no effect on markers of inflammation and oxidation
https://pubmed.ncbi.nlm.nih.gov/34171740/
More Studies:
https://www.tctmd.com/news/help-not-harm-omega-6-pufas-linked-lower-risk-cvd-events
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.114.011590
https://pubmed.ncbi.nlm.nih.gov/24645297/
https://pubmed.ncbi.nlm.nih.gov/23464640/
https://pubmed.ncbi.nlm.nih.gov/28752873/
https://pubmed.ncbi.nlm.nih.gov/15576848/
Carnivore and Keto CVD, Cancer, and Inflammation
Article taking a critical look at low carb, high fat diets that cause malignant dyslipidemia.
High levels of low-density lipoprotein cholesterol (LDL-C) may result from the reduced clearance of LDL particles from the circulation, the increased production of their precursor, or a combination of both. The increased intake of (saturated) fat and cholesterol, combined with limited to no intake of carbohydrates and fiber, are the main features of diets linked to hypercholesterolemia.
https://pubmed.ncbi.nlm.nih.gov/36839320/
Copenhagen study that demonstrated that low TG and high HDL is better than high TGs and low HDL flawed because the high TG low HDL group had higher rates of obesity, smoking, hypertension, diabetes
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/647239
Articles demonstrating that Keto and Carnivore diets can increase inflammation.
https://pubmed.ncbi.nlm.nih.gov/31067015/
Very low carb keto diets worsen lipid panels:
Case Report: After 7 months of very low carb, keto diet LDL-C of 393 mg/dl
https://academic.oup.com/jes/article/5/Supplement_1/A37/6240267
Articles demonstrating that Keto and Carnivore increase heart disease
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.035225
https://pubmed.ncbi.nlm.nih.gov/28444290/
https://www.sciencedirect.com/science/article/pii/S2666667723000363
Articles showing keto and carnivore increase stroke rates:
https://pubmed.ncbi.nlm.nih.gov/26935118/
Keto and carnivore increase hypertension:
https://pubmed.ncbi.nlm.nih.gov/26935118/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2658466/
https://academic.oup.com/ajh/article-abstract/35/8/679/6585635
Articles showing Carnivore and Keto diets can increase cancer rates:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4698595/
https://pubmed.ncbi.nlm.nih.gov/31389007/
https://pubmed.ncbi.nlm.nih.gov/26501271/
https://pubmed.ncbi.nlm.nih.gov/24629981/
https://pubmed.ncbi.nlm.nih.gov/24122646/
Pre-Press Article at American College of Cardiology showing that Keto diets increased cardiovascular mortality by 2.18 times vs standard diet after 11.8 years of follow up.
Article showing that Keto, Low Carb, and Intermittent Fasting can lead to eating disorders:
https://link.springer.com/article/10.1007/s40519-022-01437-z
https://pubmed.ncbi.nlm.nih.gov/35999438/
https://pubmed.ncbi.nlm.nih.gov/33852677/
The Cholesterol Myth Book Debunked:
Great article discussing why the authors of the book lied, made up their own studies, excluded studies that actually tracked mortality vs LDL and admitted to lying, only to sell books. Only 9 of the 19 studies actually tracked mortality.
At least five of the study authors have previously written books questioning the links between cholesterol and heart disease. The lead author Dr Uffe Ravnskov, has written a book called ‘The Cholesterol Myths: Exposing the Fallacy that Saturated Fat and Cholesterol Cause Heart Disease’. Another of the authors, London cardiologist Dr Aseem Malhotra, is a prominent campaigner against statins.
Authors admitted they deceived on purpose to sell books:
The authors themselves said that “We may have overlooked relevant studies as we only searched PubMed” (an online search for medical publications), and they may have excluded studies that evaluated LDL-C as a risk factor for death, if the study did not mention it in the title or abstract. “We may have overlooked a small number of relevant studies because we only searched papers in English,” they added.
Red Meat and Heart Disease
Articles which demonstrate that increased red meat intake increases the risk of heart disease and other risk factors of heart disease (stroke, hypertension, heart attacks, plaque, inflammation):
https://www.ahajournals.org/doi/abs/10.1161/CIRCULATIONAHA.111.039273
https://www.ahajournals.org/doi/abs/10.1161/STROKEAHA.111.620936
https://www.ahajournals.org/doi/abs/10.1161/HYPERTENSIONAHA.117.10156
Article showing red meat intake increases Inflammation:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9194089/
Results
Among all comparisons, higher total red meat intake led to higher blood CRP concentrations [0.12 mg/L (0.04, 0.19), 28 comparisons; weighted mean difference (95% CI), random effects]. This effect of red meat on CRP was also shown in the subgroup with diagnosed diseases [0.20 mg/L (0.08, 0.32), 7 comparisons], but not in the subgroup without diagnosed diseases [−0.04 mg/L (−0.17, 0.10), 12 comparisons]. Similar effects were observed when mixed processed and unprocessed red meat intakes were categorically combined as “mixed red meat” [0.18 mg/L (0.09, 0.27), 17 comparisons], but not for higher intake of unprocessed red meat [−0.07 mg/L (−0.21, 0.07), 11 comparisons]. Higher total red meat intake did not affect CRP when consuming red meat with uncontrolled habitual diets (8 comparisons) or comparing omnivorous to vegetarian or vegan diets (2 comparisons). Blood concentrations of leptin, IL-6, TNFα, or adiponectin were not affected.
Conclusions
There is a paucity of RCT-based research on red meat intake and a complete profile of inflammatory and especially anti-inflammatory markers. Results from our meta-analyses of RCTs suggest that total and mixed, but not unprocessed, red meat intakes affected blood CRP concentrations.
Article demonstrating that inflammation and BMI may actually what makes red meat intake:
https://pubmed.ncbi.nlm.nih.gov/33648505/
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-021-01922-9 (same article, free full text)
Reducing Saturated Fat
Finland North Karelia project: Reducing saturated fat, reduced CV mortality by 84% and added 10 years to life expectancy:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7444010/
Reducing saturated fat intake reduces All Cause Mortality:
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2530902
From the article:
Findings In this cohort study that included 126 233 participants followed up for as long as 32 years, higher intakes of saturated fat and trans-fat were associated with increased mortality, whereas higher intakes of polyunsaturated (PUFA) and monounsaturated (MUFA) fatty acids were associated with lower mortality. Replacing 5% of energy from saturated fats with equivalent energy from PUFA and MUFA was associated with reductions in total mortality of 27% and 13%, respectively.
Meaning These findings support current dietary recommendations to replace saturated fat and trans-fat with unsaturated fat.
Reducing saturated fat reduces all cause mortality (free pdf):
From the Article:
We identified 32 publications providing 34 data sets of SFA intakes and all-cause mortality. Data were available on 256 508 deaths in 1 509 268 people. Primary analyses relating to all-cause mortality are shown in Table 1, and replacement analyses of self-reported dietary intakes of SFA and all-cause mortality in Fig. 2. Additional analyses are shown in Annex 3.
Higher reported intakes of SFA were associated with increased risk of premature mortality when compared with lower intakes, and when comparing dietary intakes above and below 10%TE. Fewer data were available regarding the source of SFA and tissue measurements, and there was no evidence of a dose–response effect. Reductions in risk of all-cause mortality were observed in analyses where dietary SFA was replaced by PUFA, MUFA (especially plant MUFA) or carbohydrates. Replacements of SFA with MUFA from animal sources or TFA were not associated with a change in the all-cause mortality rate.
https://www.who.int/publications/i/item/9789240061668
Reducing saturated fat intake increases LDL receptors:
In summary, reducing dietary saturated fat is associated with an increase in LDL-receptor abundance of magnitude similar to the decrease in serum LDL-cholesterol. Thus, an important mechanism by which reductions in dietary saturated fatty acids decrease LDL-cholesterol in humans is through an increase in LDL-receptor number.
https://pubmed.ncbi.nlm.nih.gov/9101427/
A meta analysis of 15 studies and nearly 60,000 participants demonstrating dose response to reduction in saturated fat intake. Reducing saturated fat, lowered CVD event risk by 21%. Reducing saturated fat, reduced serum cholesterol and LDL which directly correlated with reduced CVD events and mortality:
https://pubmed.ncbi.nlm.nih.gov/32428300/
And the revised edition of that study:
https://pubmed.ncbi.nlm.nih.gov/32827219/
And original publication:
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD011737.pub2/full
Another meta analysis of 16 trials showed a 17% reduction in CV events
https://pubmed.ncbi.nlm.nih.gov/32827219/
A few more trials:
https://pubmed.ncbi.nlm.nih.gov/26068959/
https://pubmed.ncbi.nlm.nih.gov/22592684/
https://pubmed.ncbi.nlm.nih.gov/27224282/
https://journals.sagepub.com/doi/10.1177/1753944717742549
https://pubmed.ncbi.nlm.nih.gov/24034567/
In the 24-year Cohort Health Professionals Follow-Up Study (HPFS) and the 22-year and 20- year cohort NHS I and II, dairy fat consumption was not associated with the risk of total CVD. Isocaloric replacement of 5% energy from dairy fat by polyunsaturated fats (PUFA) or vegetable fat was associated with 24% and 10% reductions in CHD risk, respectively.
https://pubmed.ncbi.nlm.nih.gov/27557656/
A study by Jakobsen and colleagues of 11 US and European cohort studies showed similar results by replacing SFA with PUFA and the risk of CHD. During a 4–10 year follow up a 5% lower energy intake from SFA with an isocaloric intake from PUFA significantly reduced coronary events by 13% and coronary deaths by 26%.
https://pubmed.ncbi.nlm.nih.gov/19211817/
The 10-year Multi-Ethnic Study of Atherosclerosis (MESA) demonstrated that SFA from meat had a higher risk for CVD: hazard ratio (HR) (95% confidence interval [CI]) for +5 g/day (1.26 (1.02, 1.54) and a +5% of energy from meat SFA (1.48 (0.98, 2.23).
https://pubmed.ncbi.nlm.nih.gov/22760560/
In the 24-year Cohort Health Professionals Follow-Up Study (HPFS) and the 22-year and 20- year cohort NHS I and II, dairy fat consumption was not associated with the risk of total CVD. Isocaloric replacement of 5% energy from dairy fat by polyunsaturated fats (PUFA) or vegetable fat was associated with 24% and 10% reductions in CHD risk, respectively.
https://pubmed.ncbi.nlm.nih.gov/27557656/
Post prandial responses to butter vs olive oil in young lean men
Conclusions: Olive oil induced lower triacylglycerol concentrations and higher HDL-cholesterol concentrations than butter, without eliciting differences in concentrations of glucose, insulin, or fatty acids. Furthermore, olive oil induced higher concentrations of GLP-1 and GIP than did butter, which may point to a relation between fatty acid composition, incretin responses, and triacylglycerol metabolism in the postprandial phase.
https://pubmed.ncbi.nlm.nih.gov/10357731/
Coconut Oil Effect on Heart Disease and CVD Risk
Coconut oil significantly raises LDL cholesterol and HDL:
https://pubmed.ncbi.nlm.nih.gov/31928080/
Butter increased LDL cholesterol more than coconut oil:
https://pubmed.ncbi.nlm.nih.gov/29511019/
Replacing coconut oil with polyunsaturated fats, altered blood lipids in a manner with reduced cardiovascular risk:
https://pubmed.ncbi.nlm.nih.gov/26946252/
Fish Oil?
Eicosapentaenoic acid- REDUCE IT Trial
Used inflammatory mineral oil as placebo? Interfered with statin absorption?
- https://www.jwatch.org/na55103/2022/07/14/reduce-it-trial-result-doubt
- https://www.ajmc.com/view/reduce-it-vs-strength-still-missing-pieces-in-the-omega-3-puzzle
- https://www.ajmc.com/view/with-no-end-in-sight-on-omega-3-debate-nissen-calls-for-more-trials
- https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.122.059410
STRENGTH Trial was DHA and EPA
- Increases LDL
- No effect on CV outcomes
- Corn oil placebo, neutral?
- 69% increase in Afib
- More studies needed comparing EPA vs DHA vs Both
- And Corn Oil vs Mineral Oil
Nissen was blunt. “Fish oils increase the risk of atrial fibrillation substantially, and there is no solid evidence that they help the heart in anyway,” Nissen said in a statement. “It’s a sad story for cardiology.”
Largest Fish Oil study ever done:
https://pubmed.ncbi.nlm.nih.gov/30019766/
Good Summary of all studies on Fish Oil:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8211000/
Fish Oil and Afib
Study showing fish oil supplementation increased risk of atrial fibrillation
https://pubmed.ncbi.nlm.nih.gov/34612056/
Vitamin E Supplementation Increases All Cause Mortality
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1479533/
Calories and Weight Loss
Weight Loss in Diabetics vs Non Diabetics on low car or balanced diet:
CONCLUSIONS: There is probably little to no difference in weight reduction and changes in cardiovascular risk factors up to two years' follow-up, when overweight and obese participants without and with T2DM are randomised to either low-carbohydrate or balanced-carbohydrate weight-reducing diets.
https://pubmed.ncbi.nlm.nih.gov/35088407/
DIETFITS Trial
Trial funded by Keto and Low Carb evangelists, Gary Taubes, Peter Attia (at the time, has since changed his mind), hired lead investigator Kevin Hall. Very well done metabolic ward study.
Conclusions and Relevance In this 12-month weight loss diet study, there was no significant difference in weight change between a healthy low-fat diet vs a healthy low-carbohydrate diet, and neither genotype pattern nor baseline insulin secretion was associated with the dietary effects on weight loss. In the context of these 2 common weight loss diet approaches, neither of the 2 hypothesized predisposing factors was helpful in identifying which diet was better for whom.
https://jamanetwork.com/journals/jama/fullarticle/2673150
A huge umbrella study looking at all different diets and whether or not specific diets were better for diabetics. Regardless of which diet they followed, all diabetics lost the same amount of weight and regressed their diabetes if the diet was calorie restricted.
https://pubmed.ncbi.nlm.nih.gov/34796367/
Low carb vs balanced carb diets showed no difference CV risk or weight loss at 2 years:
There is probably little to no difference in weight reduction and changes in cardiovascular risk factors up to two years' follow‐up, when overweight and obese participants without and with T2DM are randomised to either low‐carbohydrate or balanced‐carbohydrate weight‐reducing diets.
https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD013334.pub2/full
Chinese men lose 45kg (100 pounds) eating only rice and improve all health markers:
https://pubmed.ncbi.nlm.nih.gov/1200726/
Articles demonstrating that weight loss depends on energy balance only (calories) and that macronutrient composition does not matter at all.
Obesity Energetics: Body Weight Regulation and the Effects of Diet Composition
https://pubmed.ncbi.nlm.nih.gov/28193517/
Low Fat was actually superior to low carb. Take a look at the graph from this study.
New England Journal of Medicine from 2009:
Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates
They compared diets with varying amounts of fats, carbohydrates, and protein. They found that regardless of which macronutrients were emphasized, the weight loss alone was responsible for all of the health benefits. So whether you ate mostly carbs, mostly fat, mostly protein, if you were in a calorie deficit and lost weight, your health markers all improved.
Conclusions: Reduced-calorie diets result in clinically meaningful weight loss regardless of which macronutrients they emphasize.
https://pubmed.ncbi.nlm.nih.gov/19246357/
Study from 2004 titled, A randomized trial comparing low-fat and low-carbohydrate diets matched for energy and protein, they concluded...
Our results showed no significant weight loss, lipid, serum insulin, or glucose differences between the two diets. Lipids were dramatically reduced on both diets, with a trend for greater triglyceride reduction on the VLC (very low carb) diet. Glucose levels were also reduced on both diets, with a trend for insulin reduction on the VLC diet. Compliance was excellent with both diets, and side effects were mild, although participants reported more food cravings and bad breath on the VLC diet and more burping and flatulence on the LF (low fat) diet.
The low carb group had more carvings and more disordered eating, but the very low carb and the low fat groups both lost the same amount of weight when calories were the same.
https://pubmed.ncbi.nlm.nih.gov/15601961/
Article demonstrating that proteins and fats have a greater thermic effect of food than fat:
The Thermic Effect of Food: A Review
https://pubmed.ncbi.nlm.nih.gov/31021710/
Mediterranean Diet
Articles showing that the Mediterranean Diet has cardiovascular benefits, reduces heart disease, stroke, CVD risk factors, mortality:
Lyon Diet Heart Study:
Benefit of Mediterranean diet for secondary prevention of heart disease
https://www.ahajournals.org/doi/full/10.1161/01.cir.103.13.1823
Vegetarian and vegan diets: benefits and drawbacks
https://academic.oup.com/eurheartj/advance-article-abstract/doi/10.1093/eurheartj/ehad436/7224412
Oslo Diet Heart Study, looked at 412 men after first MI and switched them from sat fat to PUFAs, had significant reduction in fatal mi, nonfatal mi, chd mortaility, all cause mortality
https://www.ahajournals.org/doi/10.1161/01.CIR.42.5.935
Lyon Diet Heart Study had similar secondary prevention outcomes wit 50-70% lower risk of recurrent disease, cardiac death, nonfatal mi, UA, stroke, chf, dvt, PE.
https://www.ahajournals.org/doi/10.1161/01.CIR.103.13.1823
Mediterranean diet reduces cardiovascular mortality by 45%, beats other popular heart healthy diets
Plant-based diets have become increasingly popular thanks to their purported health benefits and more recently for their positive environmental impact. Prospective studies suggest that consuming vegetarian diets is associated with a reduced risk of developing cardiovascular disease (CVD), diabetes, hypertension, dementia, and cancer. Data from randomized clinical trials have confirmed a protective effect of vegetarian diets for the prevention of diabetes and reductions in weight, blood pressure, glycosylated haemoglobin and low-density lipoprotein cholesterol, but to date, no data are available for cardiovascular event rates and cognitive impairment, and there are very limited data for cancer. Moreover, not all plant-based foods are equally healthy. Unhealthy vegetarian diets poor in specific nutrients (vitamin B12, iron, zinc, and calcium) and/or rich in highly processed and refined foods increase morbidity and mortality.
https://www.bmj.com/content/380/bmj-2022-072003
CARDIOPREV study:
In secondary prevention, the Mediterranean diet was superior to the low-fat diet in preventing major cardiovascular events. Our results are relevant to clinical practice, supporting the use of the Mediterranean diet in secondary prevention.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(22)00122-2/fulltext
PERIMED Trial of over 7000 people demonstrated that a Mediterranean style diet supplemented with either olive oil or nuts, resulted in a 28-30% reduction in primary end points (myocardial infarction, stroke, or death from cardiovascular causes):
https://www.nejm.org/doi/full/10.1056/nejmoa1200303
NEJM study with 7447 participants showed 30% MACE reduction in primary prevention:
https://www.nejm.org/doi/10.1056/NEJMoa1200303
Study with 1.5 million participants showed 9% reduction in CVD mortality:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4339461/
Study with 7000 participants showed 30% lower risk of MACE:
https://www.nejm.org/doi/full/10.1056/nejmoa1800389
Study of over 5000 showed 20% lower risk of MACE:
https://www.acc.org/about-acc/press-releases/2015/03/04/16/36/mediterranean-diet-cuts-heart-disease-risk-by-nearly-half
Study of 1.8 Million showed 9% lower cancer:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770822/
Study of 4000 women showed 30% reduction in breast cancer:
https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/2434738
Study of 1500 had higher survival rates after breast cancer:
https://pubmed.ncbi.nlm.nih.gov/33396551/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6770822/
Study of over 2 Million showed reduced colorectal, gastric, breast, liver, head and neck, and prostate cancer:
https://pubmed.ncbi.nlm.nih.gov/28954418/
Statins Effects and Side Effects
Study of over18,000 showing no dementia from statins:
https://pubmed.ncbi.nlm.nih.gov/34167639/
Study of over 23,000 showed no dementia and improvement of cognitive function:
https://pubmed.ncbi.nlm.nih.gov/24095248/
Article showing no new incidence of diabetes on statins, but may lead to slight worsening due to living longer and natural progression of diabetes:
https://pubmed.ncbi.nlm.nih.gov/34605849/
Jupiter trial looking at diabetes in statin treated arm, showed minimal increase in diabetes, but not very dissimilar to placebo:
https://pubmed.ncbi.nlm.nih.gov/22883507/
Jupiter Primary Prevention Trial showed people with normal LDL (below 130) and CRP over 2 showed significant reduction in mortality, MACE, CVD, and all endpoints. It showed a 44% reduction in primary endpoint, 54% reduction in heart attacks, 48% reduction in strokes, 47% reduction in the need for stents (PCI), and 20% reduction in all cause mortality. Had to be stopped early because it was unethical to not treat the placebo group:
https://pubmed.ncbi.nlm.nih.gov/18997196/
https://www.nejm.org/doi/full/10.1056/NEJMoa0807646 (full text, worth reading)
NASH (Fatty Liver) Caused by Saturated Fat, Not Sugar
Multiple studies have now demonstrated that it's increased in saturated fat intake that causes Nonalcoholic Steatohepatitis, not sugar. Many of these Medfluencers and diet gurus try to blame sugar, we have evidence to the contrary.
https://pubmed.ncbi.nlm.nih.gov/32165444/
Conclusions: Consumption of an SFA diet had a potent effect, increasing IHTAG together with exaggerating postprandial glycemia. The SUGAR diet did not influence IHTAG and induced minor metabolic changes. Our findings indicate that a diet enriched in SFA is more harmful to metabolic health than a diet enriched in free sugars.
Sugar Intake Is Going Down, Not Up
Articles demonstrating that while sugar intake has decreased over the years, obesity continues to rise:
Worldwide trends in dietary sugars intake
https://pubmed.ncbi.nlm.nih.gov/25623085/
Trends in dietary carbohydrate consumption from 1991 to 2008 in the Framingham Heart Study Offspring Cohort
https://pubmed.ncbi.nlm.nih.gov/24661608/
Trends in sugar-sweetened beverage consumption among youth and adults in the United States: 1999-2010
https://pubmed.ncbi.nlm.nih.gov/23676424/
Fat, Not Sugar, Contributed Most to Weight Gain
Articles demonstrating that the biggest contributor to the increase in caloric intake over the years has been fat, not sugar. Along with the graph showing the composition of diets from 1970 compared to 2010.
What’s on your table? How America’s diet has changed over the decades
Section 4
Articles demonstrating that differences in glycemic load do not affect weight loss or gain when calories are equated.
Effect of Low-Fat vs Low-Carbohydrate Diet on 12-Month Weight Loss in Overweight Adults and the Association With Genotype Pattern or Insulin Secretion: The DIETFITS Randomized Clinical Trial
https://pubmed.ncbi.nlm.nih.gov/29466592/
No difference in body weight decrease between a low-glycemic-index and a high-glycemic-index diet but reduced LDL cholesterol after 10-wk ad libitum intake of the low-glycemic-index diet
https://pubmed.ncbi.nlm.nih.gov/15277154/
Metabolic and behavioral effects of a high-sucrose diet during weight loss
https://pubmed.ncbi.nlm.nih.gov/9094871/
Randomized controlled trial of changes in dietary carbohydrate/fat ratio and simple vs complex carbohydrates on body weight and blood lipids: the CARMEN study. The Carbohydrate Ratio Management in European National diets
https://pubmed.ncbi.nlm.nih.gov/11093293/
Metabolic and behavioral effects of a high-sucrose diet during weight loss
https://pubmed.ncbi.nlm.nih.gov/9094871/
The effects of four hypocaloric diets containing different levels of sucrose or high fructose corn syrup on weight loss and related parameters
https://pubmed.ncbi.nlm.nih.gov/22866961/
Treatment of massive obesity with rice/reduction diet program. An analysis of 106 patients with at least a 45-kg (100 pounds) weight loss
https://pubmed.ncbi.nlm.nih.gov/1200726/
Section 5
Articles showing that sugar does not cause fat gain unless also accompanied by an increase in calories.
Dietary sugars and body weight: systematic review and meta-analyses of randomised controlled trials and cohort studies
https://pubmed.ncbi.nlm.nih.gov/23321486/
Section 6
Articles demonstrating that low carb diets do not cause more weight loss than low fat/high carb diets when calories and protein are equated.
Ketogenic low-carbohydrate diets have no metabolic advantage over nonketogenic low-carbohydrate diets
https://pubmed.ncbi.nlm.nih.gov/16685046/
Energy expenditure and body composition changes after an isocaloric ketogenic diet in overweight and obese men
https://pubmed.ncbi.nlm.nih.gov/27385608/
Low carbohydrate versus isoenergetic balanced diets for reducing weight and cardiovascular risk: a systematic review and meta-analysis
https://pubmed.ncbi.nlm.nih.gov/25007189/
Section 7
Articles demonstrating that insulin levels do not predict weight gain.
The entero-insular axis and adipose tissue-related factors in the prediction of weight gain in humans
https://pubmed.ncbi.nlm.nih.gov/17130851/
Section 8
Articles showing that overfeeding carbohydrates or fats are both equally fattening in humans.
Fat and carbohydrate overfeeding in humans: different effects on energy storage
https://pubmed.ncbi.nlm.nih.gov/7598063/
Effects of isoenergetic overfeeding of either carbohydrate or fat in young men
https://pubmed.ncbi.nlm.nih.gov/11029975/
Section 9
Article showing that NNS (non nutritive sweeteners), zero calorie sweeteners, caused more weight loss than when compared to water. Very well done study.
https://pubmed.ncbi.nlm.nih.gov/26708700/
The NNS group lost more weight and kept almost all of it off.
Section 10
Articles demonstrating that seed oils and linoleic acid are not pro inflammatory in humans and actually reduce cardiovascular mortality.
https://pubmed.ncbi.nlm.nih.gov/24645297/
https://pubmed.ncbi.nlm.nih.gov/28752873/
https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.118.038908
https://pubmed.ncbi.nlm.nih.gov/15576848/
(LA does not convert to AA in humans)
https://pubmed.ncbi.nlm.nih.gov/18990555/ (the more linoleic acid to consume, the less inflammation)
For an easy-to-read article on this that is not in a scientific journal:
https://abbylangernutrition.com/learning-curve-are-seed-oils-harmful/
Who is Dr. Alo?
I've Been Teaching Doctors Weight Loss for Over 20 Years! I'm a Board Certified Cardiologist and Certified Personal Trainer!
I've been teaching doctors how to teach their patients to lose weight properly for over 20 years. I have traveled the world teaching physicians about proper weight loss. My lectures and techniques have led to hundreds, if not thousands, of patients and clients FINALLY learning to lose weight correctly, without restrictive, outrageous diets that are sometimes dangerous.
Do you want to learn from The Doctor's Doctor who has been teaching proper weight loss for over 20 years? Or from a newly graduated, inexperienced fitness trainer?
Like everyone, I have been overweight and sometimes obese since college. I have tried almost every fad diet you can imagine; Atkins, South Beach, Sugarbusters, Zone, Nutrisystem, Weight Watchers, Whole 30, Intermittent Fasting, Keto, Paleo, TB12, and so many others. I would lose a little bit of weight, only to gain it all back. What gives? It was frustrating! I developed horrible relationships with food and exercise.
It was so embarrassing. Especially because I was "The Weight Loss Doctor" and the obesity specialist. If anyone should know how to lose weight, it should be me!
It took me over 20 years of researching and lecturing on weight loss to finally figure it out. I have read every book and research article on obesity and weight loss, and I have finally figured it out. My patients and clients love my system and how easy it is! You get to eat whatever you want, and still lose weight! And it's backed by actual research and science! You will get a copy of every single relevant study!
I'm a cardiologist and certified personal trainer, and I have been able to help thousands of my clients and patients lose weight, and they have all been asking me to make my system available for all, so I finally decided to write this book and give it away for peanuts online.
In case you are wondering, yes, that's me after losing 50 pounds of fat and gaining a bunch of muscle. It took me about 6 months. Yes, I was eating whatever I wanted. You can learn how to do this too! I reveal all of the tips and tricks and science behind my plan in my new book!
*Individual results may vary. Results not typical.

$5 Weight Loss Books
For less than 5 dollars, you can grab one of Dr. Alo's weight loss books. Includes special bonuses and the audio book! Over 20 years of practical weight loss research packed into easy to read books with a very simple weight loss plan!
Actual Weight Loss Book
The Complete Guide to Safe, Effective, Permanent, No Fad Diet, No Gimmicks, Weight Loss! (Hint: Less than $5)
The Mommy Body Makeover Book
Twenty years of research and helping busy moms lose weight, in one quick book! (Hint: Less than $5)
Special Offers On All Courses and Coaching Programs
Because you have been a loyal customer and have enjoyed our previous content, we are offering you these deals at a huge discount.

Weight Loss 101 Masterclass
Lose weight without restrictive dieting. Eat anything you want, skip the gym, and still lose weight! Learn at your own pace on your computer or on a phone app! Build a lean, toned body without avoiding foods you enjoy! While developing a good relationship with food and exercise!
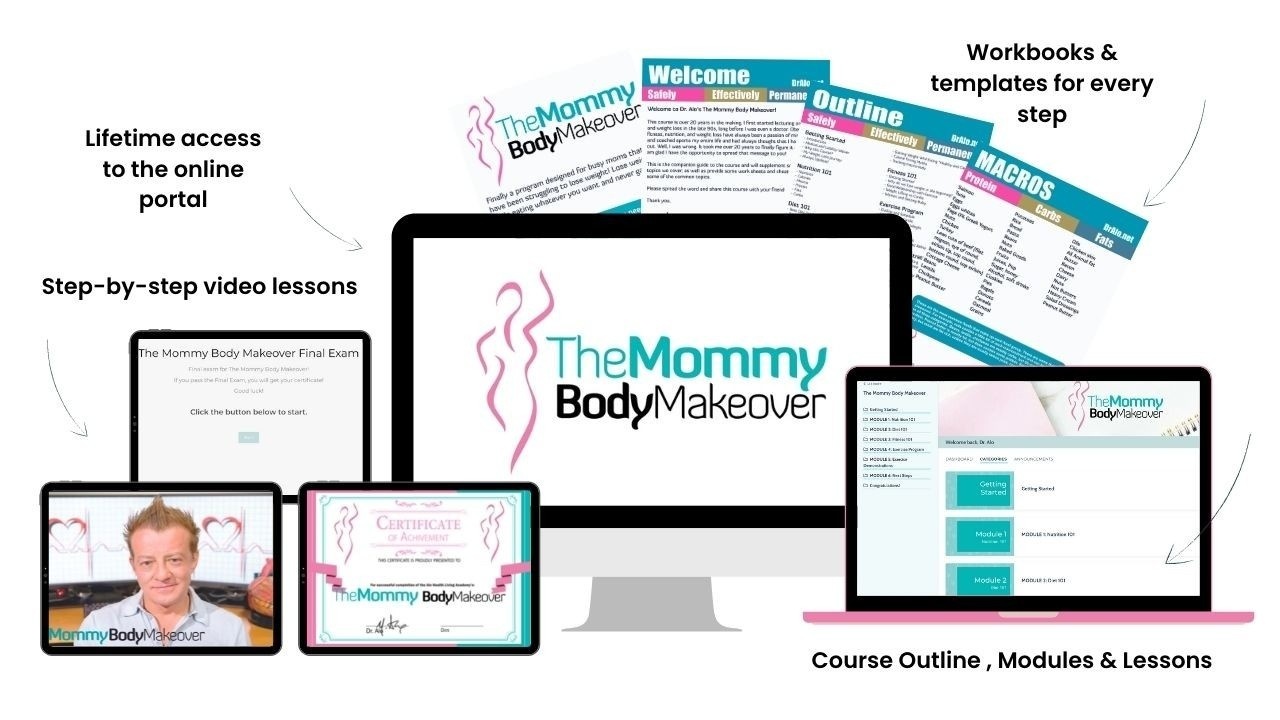
The Mommy Body Makeover Weight Loss Course
The perfect weight loss program for busy moms that want their confidence and body back! Learn at your own pace on your computer or on a phone app! No more avoiding foods! Develop a good relationship with food!

Mindset Full Course
Having a positive mindset when it comes to losing weight, health, and fitness is paramount! You can't do anything without the proper mindset! Apply neurolinguistic programming and neurocognitive techniques to get in the right state of mind for weight loss.

All of My FREE Resources and Guides!
Want more diet research, free reports, recipes, cookbooks, workbooks, cheatsheets, and guides! This is a valuable resource! Send all your friends to this link as well!
