Why Veins Don't Get Heart Disease?
Feb 14, 2026
Why Arteries Get Atherosclerosis and Not Veins?
Many people online ask this question. If LDL particles trafficking cholesterol cause atherosclerosis, why don’t veins get atherosclerosis? If LDL-C is the cause, and LDL particles are circulating in plasma, even on the venous side, why don’t veins get atherosclerosis?
Smart question, right?
No. This is another case of these Medfluencers just not knowing enough.
Arteries And Veins Are Structurally Very Different
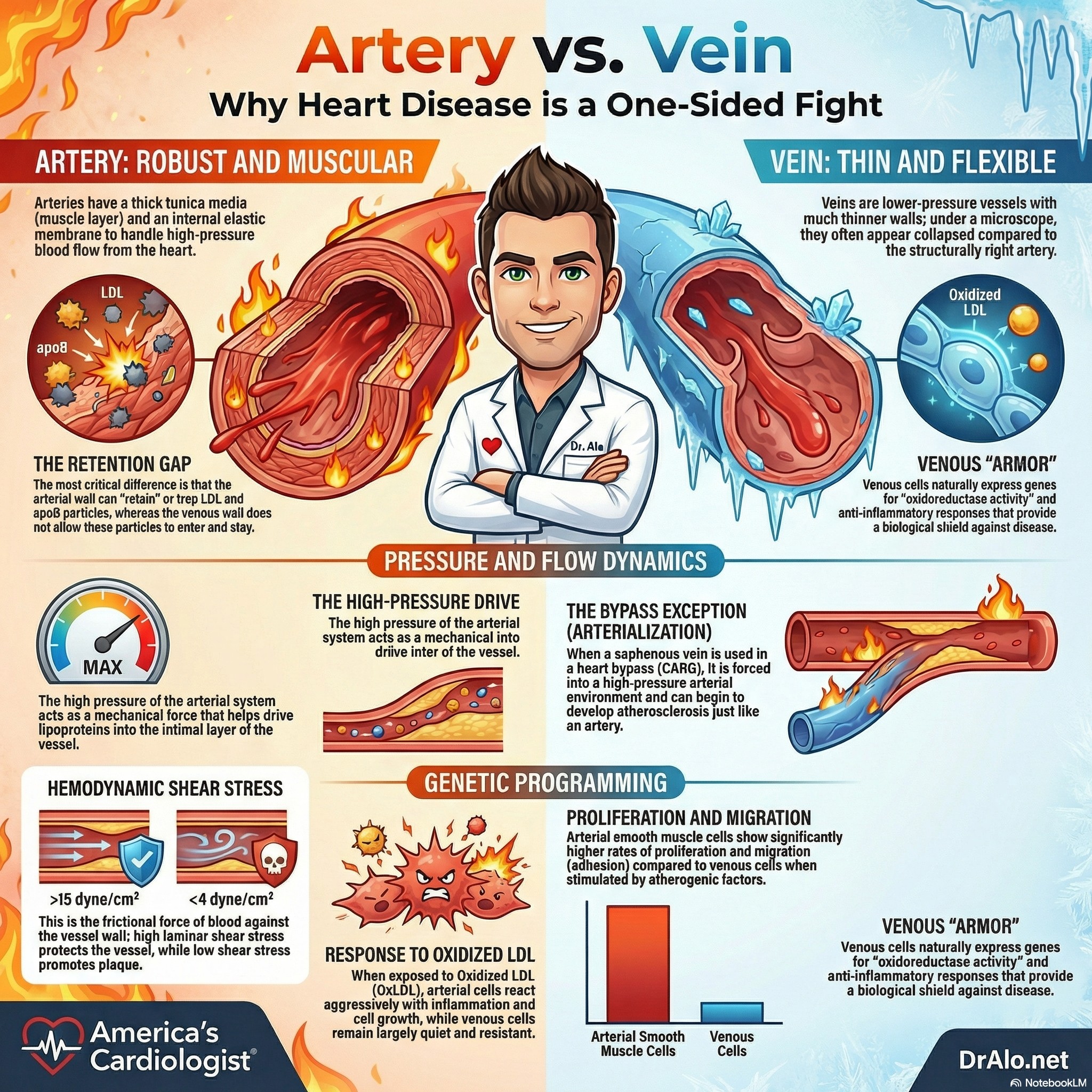
Arteries and veins are very different. Arteries are thicker, they have multiple layers, they have a muscle layer. They are not veins. Veins are thinner and composed of very different materials. They are not interchangeable. Arteries are also a higher-pressure system, which can drive lipoproteins into the intimal layer.
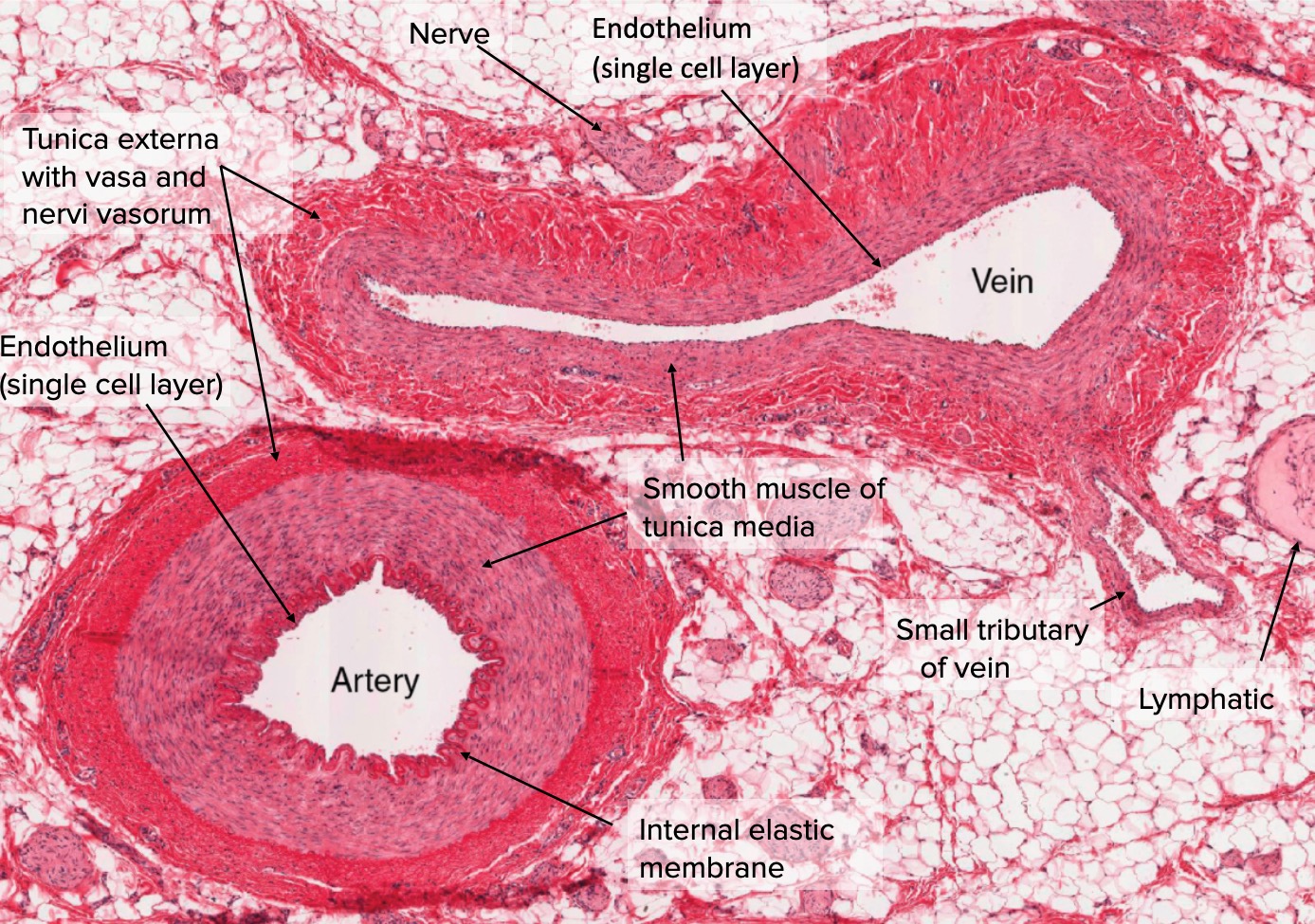
The above is a slide of an artery and a vein side by side under a microscope. Notice the vein is collapsed and the artery is held open. The artery is a higher-pressure system and has muscle, which helps keep it open. It’s more robust and has more layers than a vein. Medfluencers like to deny this fact and use cartoon models to illustrate how similar they are. They really aren’t.
Why Veins Don't Get Atherosclerosis: The Science Behind Vascular Disease Patterns
If you've ever wondered why heart attacks and strokes involve blocked arteries but not veins, you're asking one of the most fundamental questions in cardiovascular medicine. Despite being exposed to the same blood, the same cholesterol levels, and the same risk factors like smoking and diabetes, veins almost never develop atherosclerosis. The answer lies in a fascinating combination of physics, biology, and developmental programming.
The Pressure Difference
The most obvious difference between arteries and veins is pressure. Arteries operate under high pressure—your blood pressure reading of 120/80 mmHg reflects the force in your arteries. Veins, by contrast, operate in a low-pressure system, typically under 10 mmHg.
But it's not just about high versus low pressure. It's about the specific patterns of blood flow and the forces they create on vessel walls. Scientists call this force "shear stress"—essentially the friction of blood flowing against the vessel lining.
Here's where it gets interesting: atherosclerosis doesn't develop in areas of high shear stress. Instead, plaques form precisely where blood flow becomes turbulent, slow, or oscillating—typically at branch points and curves in arteries. Studies have measured shear stress at these vulnerable spots at around ±4 dyne/cm², compared to greater than 12 dyne/cm² in protected arterial regions.
Veins experience uniformly low shear stress throughout. Paradoxically, this consistent low-pressure, low-shear environment may actually protect them from the inflammatory cascade that initiates atherosclerosis in arteries.
Arteries and Veins Are Built Differently From the Start
Even before birth, your body knows which blood vessels will become arteries and which will become veins. During embryonic development, specific genes activate in arterial cells (like Notch1/4 and EphrinB2) while different genes activate in venous cells (like COUP-TFII and EphB4). This isn't just a labeling system—it fundamentally programs how these cells will behave for the rest of your life.
When researchers exposed arterial and venous endothelial cells (the cells lining blood vessels) to oxidized LDL—one of the key triggers of atherosclerosis—the responses were dramatically different. Arterial cells showed massive activation of genes related to inflammation, cell adhesion, proliferation, and cell death. Venous cells? Barely a response.
This suggests that even if you could somehow expose veins to arterial-level pressure and cholesterol, they might still resist atherosclerosis because they're molecularly programmed differently.
The Smooth Muscle Story
The cells beneath the vessel lining—vascular smooth muscle cells—also behave differently depending on whether they come from arteries or veins. When scientists compared smooth muscle cells from atherosclerotic arteries to those from veins, the arterial cells showed significantly greater proliferation, adhesion, and migration.[4]
These are exactly the cellular behaviors that drive the formation of atherosclerotic plaques. The arterial smooth muscle cells seem primed for the hyperplastic (overgrowth) responses that characterize atherosclerosis, while venous cells remain relatively quiescent.
What Happens When Veins Face Arterial Conditions?
There's a natural experiment that tests these theories: vein grafts used in bypass surgery. When surgeons use a saphenous vein from your leg to bypass a blocked coronary artery, that vein suddenly experiences arterial pressures and flow patterns.
And what happens? The vein often develops atherosclerosis-like disease over time. This suggests that while veins have some intrinsic protection, hemodynamic forces play a crucial role. The combination of low pressure and intrinsic cellular resistance likely explains why veins in their natural environment remain disease-free.
Veins Perfect Storm Of Protection
Veins don't develop atherosclerosis because of a perfect storm of protective factors: low-pressure hemodynamics that avoid the turbulent flow patterns that trigger inflammation, intrinsic cellular programming established during development that makes venous cells less responsive to atherogenic stimuli, and smooth muscle cells that don't exhibit the proliferative behavior necessary for plaque formation.
Understanding these differences isn't just academically interesting—it has practical implications for designing better vascular grafts, developing targeted therapies, and understanding why certain interventions work in arteries but not in veins, or vice versa.
The next time you look at an anatomy diagram showing the red arteries and blue veins, remember: they're not just different colors on a chart. They're fundamentally different organs, built from different molecular blueprints, operating under different physical laws, and destined for different diseases.
So Why Do Arteries Get ASCVD And Not Veins?
Arteries can retain LDL particles. Veins cannot. It’s that simple.
One interesting fact, when veins are removed from the venous side and placed into the arterial side, they can “arterialize” and can develop ASCVD. This happens when a patient undergoes coronary artery bypass surgery (CABG). Veins are used to bypass plugged up arteries and they will arterialize and can later develop ASCVD and need stents or repeat CABG. The only way to prevent this is to lower LDL-C to target levels, likely below 55 or 40 mg/dL in these patients.
The veins are placed in a higher pressure system when they are used for bypass.
Articles discussing why arteries get ASCVD and not veins:
Response to Retention:
https://www.ahajournals.org/doi/10.1161/01.ATV.15.5.551
More up to date information in Boren article:
https://academic.oup.com/eurheartj/article/41/24/2313/5735221
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7308544/
https://journals.lww.com/co-lipidology/fulltext/2016/10000/the_central_role_of_arterial_retention_of.6.aspx
We may not fully understand the chemical signaling pathways and mechanisms, but arteries retain LDL particles and veins do not, as LDL particles do not enter veins.
References
- Hemodynamic Shear Stress and Its Role in Atherosclerosis. Malek AM, Alper SL, Izumo S. JAMA. 1999;282(21):2035-42. doi:10.1001/jama.282.21.2035.
- Shear Stress, Arterial Identity and Atherosclerosis. Lehoux S, Jones EA. Thrombosis and Haemostasis. 2016;115(3):467-73. doi:10.1160/TH15-10-0791.
- Differences in Vascular Bed Disease Susceptibility Reflect Differences in Gene Expression Response to Atherogenic Stimuli. Deng DX, Tsalenko A, Vailaya A, et al. Circulation Research. 2006;98(2):200-8. doi:10.1161/01.RES.0000200738.50997.f2.
- Vascular Smooth Muscle Cells Derived From Atherosclerotic Human Arteries Exhibit Greater Adhesion, Migration, and Proliferation Than Venous Cells. Faries PL, Rohan DI, Wyers MC, et al. The Journal of Surgical Research. 2002;104(1):22-8. doi:10.1006/jsre.2002.6399.
Still Have Questions? Stop Googling and Ask Dr. Alo.
You’ve read the science, but applying it to your own life can be confusing. I created the Dr. Alo VIP Private Community to be a sanctuary away from social media noise.
Inside, you get:
-
Direct Access: I answer member questions personally 24/7/365.
-
Weekly Live Streams: Deep dives into your specific health challenges.
-
Vetted Science: No fads, just evidence-based cardiology and weight loss.
Don't leave your heart health to chance. Get the guidance you deserve. All this for less than 0.01% the cost of health insurance! You can cancel at anytime!
[👉 Join the Dr. Alo VIP Community Today]