Heart Disease in Women: Symptoms, Tests, and Prevention Guide
Feb 07, 2026
Women and Heart Disease: The Complete Prevention Guide (Symptoms, Risks, Tests, and a Step-by-Step Plan)
By Dr. Abeer Berry DO, FACC Preventative Cardiologist Michigan
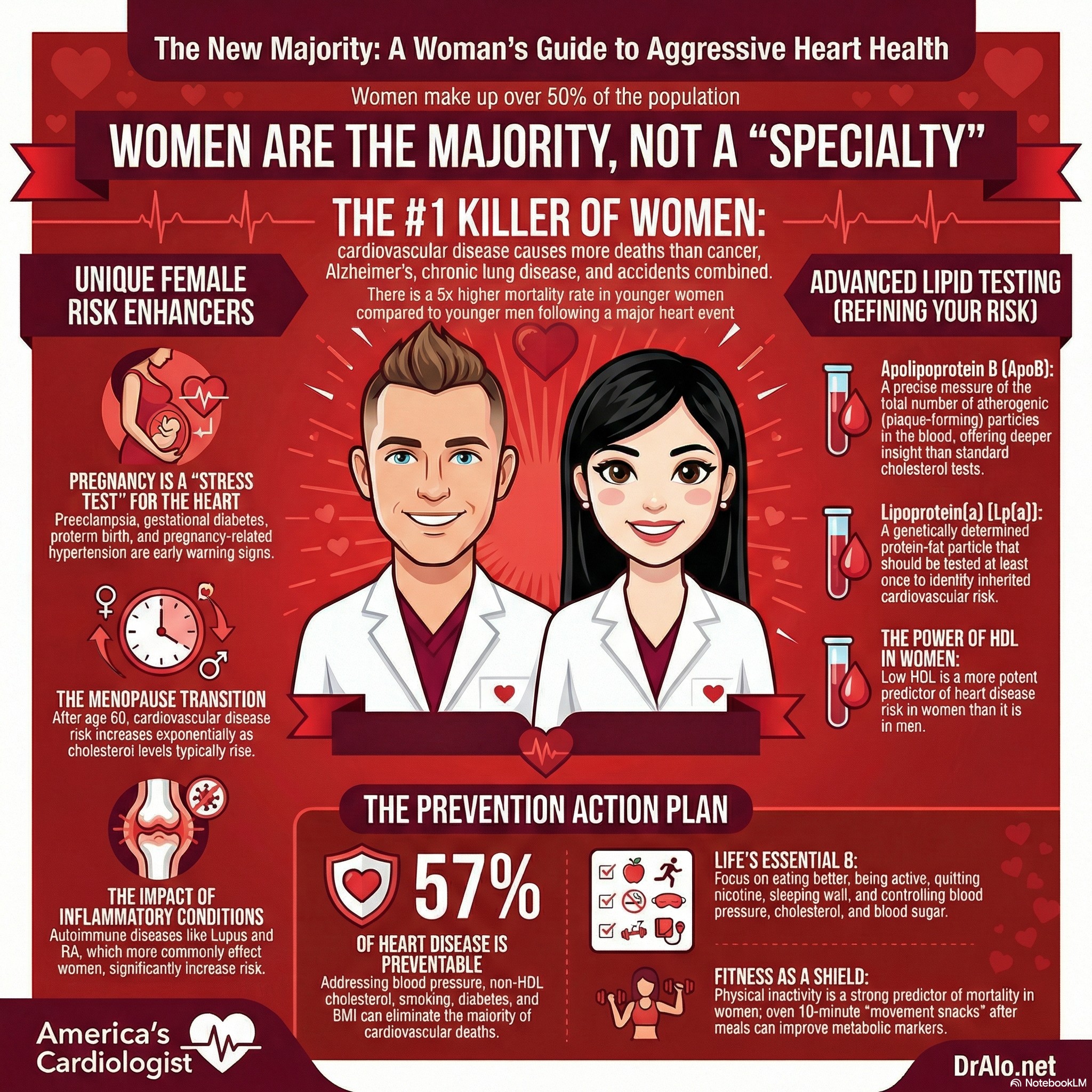
Women are the majority of patients. They are not a "specialty population". Unfortunately, for too long, we have treated women like they are an outlier or anomaly. They are not. They are the majority of people on this planet. The medical community has ignored women's health for too long.
 Dr. Abeer Berry DO, FACC |
Heart disease is the leading cause of death for women in the United States, and it can affect women at any age. Heart disease kills 1 in 3 women, whereas breast cancer kills 1 in 33 women. Yet, we spend a lot of time telling women to worry about breast cancer, when most will die to heart disease. Heart disease is completely preventable now, and we have the tools to completely eliminate this ruthless killer of women. Many women are never told their real risk until something serious happens. The goal of this guide is to change that with clear, practical steps you can use now.
This is a very deep dice into women's heart disease, we will cover everything you need in one place:
- The symptoms women notice first (and the ones that get missed)
- The biggest risk factors, including women-specific ones
- What tests to ask for and when
- Prevention that is realistic and measurable
- Medications and common concerns (statins, blood pressure meds, aspirin)
- Conditions that affect women more often, like INOCA and pregnancy-related heart risks
- Stroke and atrial fibrillation basics
- Menopause, sleep, stress, and lifestyle habits that truly move the needle
Medical safety note: This is educational. If you have urgent symptoms, talk to your doctor or call 911.
Share this with friends to spread awareness
Women & Heart Disease Topics Covered:
- The two questions most women ask
- Heart attack symptoms in women
- Heart disease symptoms that are not a heart attack
- Why women’s heart disease can look different
- The major risk factors that drive most heart disease
- Women-specific risk factors many women do not know about
- Conditions that are more common in women (INOCA, SCAD, Takotsubo, postpartum heart failure)
- A simple screening schedule: what to check and how often
- Tests to ask for (and what they mean)
- A prevention plan that actually works (Life’s Essential 8 + practical steps)
- Medications for prevention: statins, BP meds, diabetes meds, aspirin
- Atrial fibrillation and stroke prevention basics
- Menopause, hormone therapy, and heart risk
- Sleep and sleep apnea
- Stress, depression, and the heart
- A 90-day “start here” plan
- FAQs
- References
1) The two questions most women ask
“How do I know if my symptoms are my heart?”
Many women search for:
- Heart attack symptoms in women
- Heart disease symptoms in women
- “Can nausea or jaw pain be a heart attack?”
- “Is this anxiety or my heart?”
You deserve a clear answer. Start with the emergency warning signs next.
“How do I prevent heart disease before it happens?”
Prevention is not one magic supplement. It is:
- knowing your numbers
- catching women-specific risks early
- building habits that lower blood pressure, cholesterol, and blood sugar
2) Heart attack symptoms in women
Chest discomfort is still common in women. But women are also more likely to have symptoms that feel vague, unusual, or unrelated.
Common heart attack symptoms women report
- Chest pressure, squeezing, tightness, or pain
- Shortness of breath
- Pain in the arm, shoulder, back, neck, or jaw
- Nausea or vomiting
- Cold sweat
- Lightheadedness or dizziness
- Unusual fatigue that is sudden or severe
When to treat it as an emergency
Call 911 immediately if symptoms are:
- new, severe, or getting worse
- happening with exertion
- happening with sweating, nausea, or shortness of breath
- lasting more than a few minutes or coming and going
Do not drive yourself. Do not “wait to see.” Time matters.
3) Heart disease symptoms that are not a heart attack
Many women have heart disease for years before a heart attack occurs.
Symptoms that should prompt a medical evaluation
- Shortness of breath with activity, or worsening over time
- Chest tightness, heaviness, pressure, or burning
- Reduced exercise tolerance (you tire earlier than before)
- Swelling in legs or ankles
- Palpitations or a racing heartbeat
- Unexplained fatigue that persists
- Dizziness or near-fainting with exertion
If symptoms repeatedly show up with activity and improve with rest, that pattern matters.
4) Why women’s heart disease can look different
Women can develop heart disease in ways that do not always match the “classic” picture.
- Symptoms can be less dramatic.
- Some women have reduced blood flow to the heart even when major arteries look “not blocked.”
- Pregnancy history and menopause timing can change risk significantly.
- Women have been underrepresented in older research, which affected awareness and diagnosis.
This is why your story, your pregnancy history, and your lab numbers all matter.
5) The major risk factors that drive most heart disease
If you want the highest return on effort, focus on these first.
High blood pressure
High blood pressure is one of the strongest drivers of heart attack, stroke, heart failure, and kidney disease. Many women feel fine until damage has already occurred.
Action: Know your home blood pressure numbers, not just clinic readings.
High cholesterol (especially LDL and non-HDL cholesterol)
Cholesterol problems do not cause symptoms. LDL and non-HDL cholesterol are key targets in prevention discussions.
Action: Get a lipid panel and review results in the context of your overall risk.
Diabetes and prediabetes
Diabetes strongly increases cardiovascular risk. Prediabetes is a warning sign that deserves action now.
Action: Know your A1c or fasting glucose, especially if you had gestational diabetes.
Smoking and vaping
Nicotine use increases cardiovascular risk. If you use nicotine, quitting is one of the fastest ways to reduce risk over time.
Action: Use proven tools: nicotine replacement, prescription options, and coaching.
Physical inactivity and low fitness
Fitness protects the heart. It also improves blood pressure, blood sugar, triglycerides, mood, and sleep.
Action: Start with walking. Consistency beats intensity.
Weight and metabolic health
Weight alone is not the full story. Waist size, blood pressure, cholesterol, and blood sugar often explain risk better than a number on a scale.
Action: Track waist size and metabolic markers, not only weight.
6) Women-specific risk factors many women do not know about
These are often missed in routine visits, but they can change your prevention plan.
Pregnancy-related conditions (big risk clues)
If you have ever had:
- pregnancy-related high blood pressure
- preeclampsia
- gestational diabetes
- preterm birth
- small for gestational age baby
- pregnancy loss or placental complications
Your pregnancy history should be treated like an early warning system for your future heart and blood vessel health.
Action: Ask for a postpartum and long-term heart risk plan. Do not assume everything resets after delivery.
Early or premature menopause
Menopause timing matters. Earlier menopause is linked to higher cardiovascular risk, and the menopause transition can be a time when blood pressure, cholesterol, body composition, and sleep change.
Action: Treat perimenopause as a prevention window. Recheck your risk factors during this transition.
PCOS (polycystic ovary syndrome)
PCOS is often linked with insulin resistance and metabolic risk.
Action: Make sure screening includes A1c, lipids, blood pressure, and sleep.
Autoimmune and inflammatory diseases
Conditions like lupus or rheumatoid arthritis involve chronic inflammation that can raise cardiovascular risk.
Action: Prevention has to be more proactive. Control inflammation and manage traditional risk factors aggressively.
Depression and chronic stress
Depression and chronic stress are linked to worse cardiovascular outcomes and can reduce energy, sleep quality, and adherence to healthy routines.
Action: Treat mental health as part of heart prevention, not as separate.
7) Conditions that affect women more often (and get missed)
INOCA and microvascular angina
Some women have ischemia (low blood flow) and angina symptoms even when large coronary arteries do not look significantly blocked. This is often called INOCA (ischemia with non-obstructive coronary arteries) and may involve small vessel dysfunction.
Clue: Persistent chest discomfort, shortness of breath, or exertional symptoms with “normal” angiogram results.
Action: If you have ongoing symptoms, ask whether microvascular disease or INOCA has been considered and whether further functional testing is appropriate.
SCAD (spontaneous coronary artery dissection)
SCAD is a different type of heart attack mechanism involving a tear in the artery wall, and it can occur in women who otherwise seem healthy. It is often associated with the postpartum period or other hormonal transitions.
Action: If you are postpartum and have chest pain or severe symptoms, seek emergency care and make sure clinicians consider SCAD.
Peripartum cardiomyopathy (postpartum heart failure)
This is a form of heart failure that can occur late in pregnancy or in the months after delivery. It can look like normal postpartum fatigue at first.
Clues: Shortness of breath, swelling, trouble lying flat, sudden weight gain from fluid, racing heartbeat.
Action: Do not ignore these symptoms postpartum. Early evaluation is critical.
Takotsubo syndrome (broken heart syndrome)
This condition can mimic a heart attack and is often triggered by emotional or physical stress. It affects women more often than men.
Action: If symptoms feel like a heart attack, treat it like a heart attack until proven otherwise.
8) A simple screening schedule: what to check and how often
This is a reasonable starting framework for many women. Your plan may be more frequent if you have risk factors or a strong family history.
Blood pressure
- Check at least yearly in clinic
- Consider home checks if elevated, borderline, or you have pregnancy-related BP history
Lipids (cholesterol panel)
- Every 4 to 6 years for low-risk adults is common
- More often if risk factors exist, if you are in perimenopause, or if values are abnormal
Blood sugar (A1c or fasting glucose)
- Regular screening in adulthood
- Earlier and more often if overweight, have PCOS, had gestational diabetes, or have family history
Pregnancy history review
- Once postpartum and again at primary care visits
- Make sure it is documented as part of your long-term risk profile
9) Tests to ask for (and what they mean)
You do not need every test. You need the right tests based on your risk and symptoms.
The basics
- Blood pressure (home and office)
- Lipid panel (LDL, HDL, triglycerides, non-HDL) - at an LDL cholesterol level above 60 mg/dL, most people are building plaque
- A1c or fasting glucose
- Kidney function (often part of routine labs)
Risk refinement tests (when appropriate)
These tests can help if your risk is unclear or if you and your clinician are uncertain about medication decisions.
Coronary artery calcium score (CAC)
- A CT scan that measures calcified plaque in coronary arteries
- Often used to refine risk when the decision about statin therapy is uncertain
- This detects late stage heart disease and is not an early detection tool
- If you want to prevent late stage disease, treat your LDL decades before calcium develops
Lipoprotein(a), also called Lp(a)
- A genetically influenced cholesterol particle
- Many guidelines support measuring it at least once in a lifetime in higher-risk people or those with family history
Apolipoprotein B (ApoB)
- A measure related to the number of atherogenic particles
- Can help refine risk when triglycerides are high or when metabolic syndrome is present
High-sensitivity CRP (hs-CRP)
- A marker of inflammation that can contribute to risk assessment in select cases
- Is a very non-specific test and sometimes does not add much value
- Those with autoimmune and inflammatory disease may have chronically elevated levels
Symptom-based testing
If you have symptoms, the best test depends on your story and exam. Not every woman needs a treadmill test first. Some women need imaging tests, and some need evaluation for microvascular disease.
Action phrase for your appointment:
“I want to make sure we are not missing women-specific causes of chest pain and shortness of breath, including microvascular angina or INOCA. What testing is most appropriate for my situation?”
10) Women's prevention plan that actually works
A simple, high-impact approach is to use the American Heart Association’s Life’s Essential 8 as your foundation:
- Eat better
- Be more active
- Quit nicotine
- Sleep well
- Manage weight
- Control cholesterol
- Control blood sugar
- Control blood pressure
Now let’s turn that into practical steps.
Nutrition that supports heart health
You do not need perfection. You need patterns. Try to achieve 80-90% compliance. Perfection can hinder efforts.
Most evidence-based eating patterns:
- Mediterranean-style eating
- DASH-style eating
Simple rules that work:
- Build meals around vegetables, beans, lentils, fruit, whole grains
- Choose fish, poultry, and plant proteins more often
- Avoid saturated fat (butter, cheese, bacon, lard, ghee, tallow, coconut oil, fat in red meat)
- Use unsalted nuts and olive oil in reasonable amounts
- Reduce ultra-processed foods and sugary drinks
- Watch sodium if blood pressure is high
Easy plate method:
- Half plate: vegetables
- Quarter plate: lean protein
- Quarter plate: high-fiber carbs (whole grains, beans, starchy vegetables)
- Add: water, fruit, and a healthy fat
- Fat is not essential, and you can reduce it or not consume it, your body can easily make it
Exercise that improves your numbers
Aim for a mix:
- Cardio (walking counts)
- Strength training (protects metabolism, bones, and function)
- Movement snacks during the day (5 to 10 minutes helps)
If you are busy, start with:
- 10 minutes after meals, most days
- 2 short strength sessions per week
Sleep as a cardiovascular tool
Sleep affects:
- blood pressure
- appetite hormones
- insulin resistance
- inflammation
Goal: consistent sleep schedule and sufficient sleep for you.
Stress and mental health
Stress is real, and it shows up in the body. The goal is not “no stress.” It is better recovery.
Start with:
- 5 minutes of breathing or prayer/meditation daily
- walking outside
- reducing alcohol and late-night screen time
- getting support for anxiety or depression
11) Medications for prevention (clear, woman-centered guidance)
Lifestyle is the base. Medications are tools that can dramatically reduce risk when used for the right person.
Statins
Statins reduce LDL cholesterol and lower the risk of heart attack and stroke in appropriate women. Many women delay statins because of fear or mixed information online. The JUPITER trial showed a 46% reduction in heart attacks and strokes in women, in just 13 months of being on rosuvastatin.
Common questions I hear:
- “Will statins hurt my liver?”
- “Will I get muscle pain?”
- “Do I really need this?”
Balanced answer:
- Many people tolerate statins well.
- If side effects occur, dose adjustments or different statins often help.
- The decision should be based on your overall risk, not fear.
Important for women: If you are pregnant, trying to become pregnant, or could become pregnant, talk with your clinician about medication safety and planning.
Blood pressure medications
If blood pressure remains high despite lifestyle changes, medication can prevent long-term damage. The “right” medication depends on your health history and side effects.
Diabetes and metabolic medications
For some women, medications that improve blood sugar and support weight loss can also reduce cardiovascular risk. The best choice depends on your diagnosis, labs, and goals.
Aspirin (primary prevention)
Aspirin is not automatically recommended for everyone anymore. For many adults, bleeding risk can outweigh benefit. Aspirin is still used for secondary prevention in people with prior heart attack, stroke, or known vascular disease, under medical guidance.
Action: Do not start or stop aspirin without discussing your personal risk and history with your clinician.
12) Atrial fibrillation and stroke prevention basics
Atrial fibrillation (AFib)
AFib is an irregular rhythm that increases stroke risk.
Symptoms can include:
- fluttering or racing heartbeat
- shortness of breath
- fatigue
- dizziness
Some women have no symptoms and discover AFib later, which is why checkups matter.
Stroke Warning Signs in Women (F.A.S.T.)
Stroke is a medical emergency. Remember F.A.S.T.
- Face drooping
- Arm weakness
- Speech difficulty
- Time to call 911
If symptoms are sudden, treat it as an emergency.
13) Menopause, hormone therapy, and heart risk
Menopause is a transition where many risk factors can shift:
- blood pressure can rise
- LDL cholesterol can increase
- sleep can worsen
- body fat distribution can change
Hormone therapy and heart disease (HRT)
Hormone therapy can be appropriate for some women for symptom relief, and timing matters. It is not generally used as a primary tool to prevent heart disease. Decisions should be personalized based on symptoms, age, time since menopause, and medical history. See my extensive library on menopause and heart disease. Search tis blog for "menopause"
Action: If considering hormone therapy, ask for a heart-aware discussion that includes your blood pressure, lipids, blood sugar, and clot risk.
14) Sleep apnea and the heart
Sleep apnea is common and underdiagnosed, especially in women. It is linked with higher rates of high blood pressure, stroke, and coronary artery disease.
Common clues (including in women):
- loud snoring or witnessed pauses in breathing
- morning headaches
- daytime fatigue
- insomnia symptoms
- high blood pressure that is hard to control
Action: If you suspect sleep apnea, ask whether a sleep study is appropriate.
15) Stress, depression, and women's hearts
Emotional health influences:
- inflammation
- sleep
- eating patterns
- activity level
- blood pressure
Action steps that are simple and effective:
- build a daily decompression routine
- reduce nicotine and excess alcohol
- treat depression and anxiety as medical conditions, not personal failures
- ask for support early, not after burnout
16) A 90-day “start here” plan for heart Disease Prevention In Women
Week 1: Know your baseline
- Home blood pressure readings for 7 days
- Order labs: lipid panel and A1c (or fasting glucose)
- Write down pregnancy history and menopause status
- List family history of early heart disease
Weeks 2 to 4: Build your foundation
- Walk 10 minutes after one meal daily
- Add vegetables to two meals per day
- Set a consistent sleep and wake time
- If you use nicotine, set a quit plan with support
Weeks 5 to 8: Upgrade
- Increase walking to most days
- Add strength training twice per week
- Reduce sugary drinks and ultra-processed snacks
- Discuss medications if numbers remain high
Weeks 9 to 12: Personalize
- Review results with your clinician
- Decide on risk refinement tests if uncertain (CAC, Lp(a), ApoB)
- Create a long-term plan and follow-up schedule
17) FAQs For Women's Heart Disease
What are early signs of heart disease in women?
Shortness of breath with exertion, reduced exercise tolerance, chest pressure or tightness, unusual fatigue, palpitations, and swelling can all be signs. Patterns with exertion matter.
Can heart symptoms feel like anxiety or indigestion?
Yes. Symptoms can overlap. If symptoms are new, worsening, or happen with exertion, get evaluated.
What tests should I ask my doctor for?
Start with blood pressure, lipid panel, A1c, and a risk discussion that includes pregnancy history. Consider CAC, Lp(a), ApoB, or symptom-based testing when appropriate.
Do women need different prevention than men?
The basics are the same, but women have additional risk enhancers such as pregnancy complications, menopause timing, and higher likelihood of conditions like INOCA.
References On Women's Heart Disease:
- CDC. About Women and Heart Disease.
- CDC. Heart Disease Facts and Statistics.
- American Heart Association. Heart Attack Symptoms in Women.
- ACC/AHA. 2019 Guideline on the Primary Prevention of Cardiovascular Disease (Guidelines Made Simple and Executive Summary sources).
- American Heart Association. Adverse Pregnancy Outcomes and Cardiovascular Disease Risk (Scientific Statement).
- American Heart Association. Life’s Essential 8 and supporting scientific update.
- ACC. Update on Lipoprotein(a) and AHA professional toolkit on Lp(a).
- AHA. Sleep Apnea and Heart Disease/Stroke and AHA scientific statement on OSA and CVD.
- AHA. Atrial Fibrillation and stroke risk education.
- American Stroke Association. F.A.S.T. stroke warning signs.
- USPSTF. Aspirin Use to Prevent Cardiovascular Disease: Preventive Medication (2022) plus ACC summary.
- ACC/AHA. 2018 Guideline on the Management of Blood Cholesterol (Guidelines Made Simple).
- INOCA and women’s ischemic heart disease overviews.
- AHA. Coronary Artery Dissection (SCAD) and pregnancy-associated SCAD source.
- AHA. Peripartum Cardiomyopathy patient page and fact sheet.
- Menopause and cardiovascular risk: AHA scientific statement and NAMS hormone therapy position statement summaries.
- Mayo Clinic. Takotsubo (Broken Heart Syndrome) overview.
and
Still Have Questions? Stop Googling and Ask Dr. Alo.
You’ve read the science, but applying it to your own life can be confusing. I created the Dr. Alo VIP Private Community to be a sanctuary away from social media noise.
Inside, you get:
-
Direct Access: I answer member questions personally 24/7/365.
-
Weekly Live Streams: Deep dives into your specific health challenges.
-
Vetted Science: No fads, just evidence-based cardiology and weight loss.
Don't leave your heart health to chance. Get the guidance you deserve. All this for less than 0.01% the cost of health insurance! You can cancel at anytime!
[👉 Join the Dr. Alo VIP Community Today]