Does Oxidized LDL Cause Heart Disease? Myth Busting!
Feb 15, 2026
Does Oxidized LDL Cause Heart Disease?
At some point measuring oxidized LDL was discovered and there was much excitement about using that as a marker and predictor of cardiovascular outcomes.
The theory was that only oxidized (inflamed or damaged) LDL particles can cross the arterial wall and cause damage. This is not true. When present in excess concentrations, in general, all LDL particles are equally atherogenic.
Unfortunately, the data has not shown that oxidized LDL is a useful marker. This has not prevented the Medfluencer crowd from propping up the “oxLDL” as the ultimate test, mainly because they want to keep eating a high saturated fat diet, have an extremely elevated LDL cholesterol, but tell themselves it’s ok, because they are not oxidized, or they are “big and fluffy”.
Evidence That LDL Oxidation Status Does Not Predict Outcomes Nor Cause Heart Disease
Multiple lines of evidence demonstrate that LDL oxidation status does not independently affect cardiovascular outcomes when adjusted for apoB particle number. The most direct evidence comes from antioxidant trials and circulating oxLDL measurement studies.
There are many ways and angles to test this theory and prove or disprove it. Scientists have done this for us.
oxLDL Is Not An Independent Predictor After Adjusting For apoB
A large study published in the Journal of the American College of Cardiology, investigated whether measuring oxidized low-density lipoprotein (oxLDL)—a specific type of "bad" cholesterol that has undergone chemical changes—could effectively predict a person's risk for coronary heart disease (CHD). While previous research suggested that oxLDL was a strong risk factor, this study aimed to determine if it provided any unique information that wasn't already covered by standard lipid tests, such as total cholesterol, HDL ("good") cholesterol, and triglycerides. To test this, researchers analyzed blood samples and health data from over 18,000 men and 32,000 women over several years, comparing those who developed heart disease with healthy control subjects.
The researchers found that while higher levels of oxLDL were indeed linked to an increased risk of heart disease, this connection largely disappeared once they accounted for other standard health markers. Specifically, when the data was adjusted for apolipoprotein B100 (apoB)—a protein found on all potentially harmful cholesterol particles—or the ratio of total cholesterol to HDL, oxLDL was no longer a significant independent predictor of heart disease. In simpler terms, the standard tests already used by doctors were more powerful and accurate at predicting heart health than the more expensive oxLDL test. The study concluded that for the average person, there is currently no added benefit to paying for extra oxLDL testing, as it doesn't provide better information than the lipid panels already commonly available in clinical practice.
But is there any other way to prove this?
Antioxidant Supplementation Trials Show No Cardiovascular Benefit
Large-scale randomized controlled trials of antioxidant vitamins—which should prevent LDL oxidation if oxidation were causally important—have consistently failed to reduce cardiovascular events. A meta-analysis of 50 trials including 294,478 participants found that vitamin and antioxidant supplementation was not associated with reductions in major cardiovascular events (RR 1.00, 95% CI 0.98-1.02). Specifically for vitamin E, which is incorporated into LDL particles and prevents oxidation in vitro, pooled evidence from 9 RCTs (n=107,772) showed no effect on all-cause mortality (OR 1.02, 95% CI 0.97-1.07) or cardiovascular disease events (OR 0.96, 95% CI 0.90-1.04).
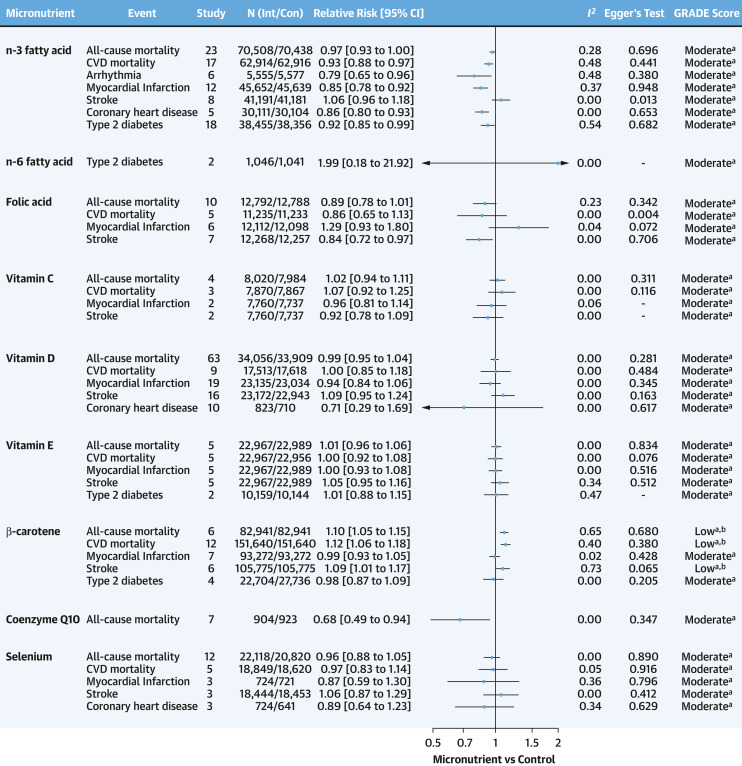
Figure 8. Effects of Antioxidant Micronutrients on Clinical CVD and T2D Risks
Micronutrient Supplementation to Reduce Cardiovascular Risk. J Am Coll Cardiol. December 12, 2022.
In another study, the Physicians' Health Study II, which randomized 14,641 male physicians to vitamin E, vitamin C, both, or placebo, found no benefit for major cardiovascular events, myocardial infarction, stroke, or cardiovascular mortality with either antioxidant alone or in combination.
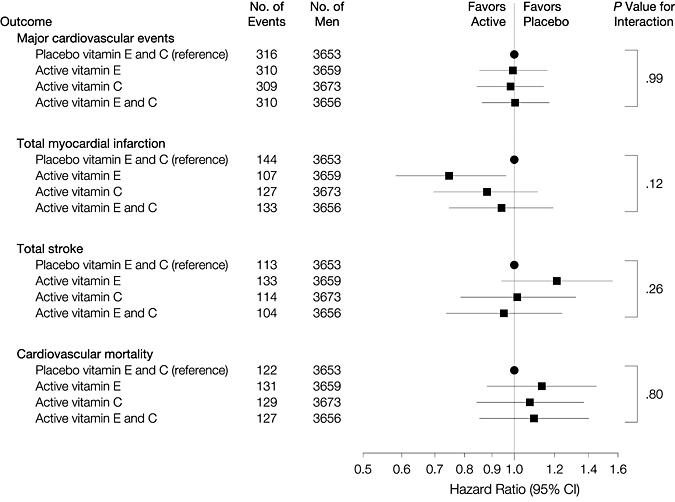
Figure 3. Hazard Ratios and 95% Confidence Intervals of Major Cardiovascular Events, Total Myocardial Infarction, Total Stroke, and Cardiovascular Mortality in the Physicians' Health Study II
Vitamins E and C in the Prevention of Cardiovascular Disease in Men: The Physicians' Health Study II Randomized Controlled Trial. JAMA. November 11, 2008.
Circulating OxLDL Does Not Predict Events Independent of ApoB
The most definitive study addressing your specific question comes from Wu et al., who examined 266 men and 235 women who developed coronary heart disease in two large prospective cohorts. When oxLDL and apoB were mutually adjusted, only apoB was predictive of CHD. The authors concluded: "circulating oxLDL, measured with antibody 4E6, is not an independent overall predictor of CHD after adjustment of lipid markers and is less predictive in development of CHD than apoB and TC/HDL-C ratio."
This finding is critical because it directly tests whether oxidation status adds information beyond particle number. It does not.
The Probucol Paradox
Probucol provides an interesting natural experiment. This drug is a potent antioxidant that dramatically reduces LDL oxidation but also lowers HDL-C by approximately 25-30%. Despite its strong antioxidant effects, the PROSPECTIVE trial (876 patients) showed only a non-significant trend toward benefit (adjusted HR 0.67, 95% CI 0.44-1.03). If LDL oxidation were the primary driver of atherosclerosis, probucol should have shown dramatic benefit—but it didn't, despite effectively preventing oxidation.
Genetic Evidence Is Mixed
Genetic studies examining variants that affect LDL oxidation susceptibility show inconsistent results. While some polymorphisms in the OLR1 gene (encoding the oxLDL receptor LOX-1) associate with cardiovascular disease, these associations are confounded by the fact that the same variants may affect other aspects of lipoprotein metabolism. [8-9] Importantly, no Mendelian randomization studies have demonstrated that genetically determined increases in LDL oxidation susceptibility cause cardiovascular disease independent of apoB levels.
The Key Distinction: Oxidation as Consequence vs. Cause
Your summary correctly identifies that oxidation occurs after retention in the arterial wall, not in circulation. This temporal sequence is crucial, oxidation amplifies the inflammatory response to retained apoB particles but is not necessary for their initial retention and trapping by proteoglycans. [10] The response-to-retention model explains why:
- ApoB particle number drives retention (concentration gradient)
- Retained particles undergo oxidation in the arterial wall
- Oxidized LDL accelerates foam cell formation and inflammation
- But preventing oxidation doesn't prevent retention or atherosclerosis
This explains why antioxidant trials failed despite oxidized LDL being abundant in plaques, the oxidation is downstream of the fundamental problem, which is too many apoB particles entering and being retained in the arterial wall.
Does Oxidation Have Any Effect On Atherogenicity or Cause Heart Disease?
Very little LDL particles are in circulation. the immune system removes them instantly. They are barely measurable. But labs jumped on this trend and started allowing people to order this investigational lab test, because they can make money on another test that is not covered by insurance. It was cash pay only, hence, they can actually make more.
Simple question...
Do you know what has nothing to do with LDL particle atherogenicity? Whether a few are oxidized. It doesn’t matter if they are oxidized or not.
Minimally oxidized LDL particles do exist in plasma in extremely small concentrations. There are a few studies linking them to ASCVD risk but in none of those studies was oxLDL adjusted for apoB.
Oxidized “anything” does not exist in circulation. Your liver and immune system will eliminate them instantaneously. But this doesn’t prevent Medfluencers from taking this concept and running with it. We realized this was not accurate back in 2005 in the cardiology world, yet these people continue to run with this wild theory.
If ordered by physicians, labs will perform the oxLDL test, but the result provides no clinically significant information. Too many Medfluencers over emphasize the role of “oxidation” of LDL particles.
However, LDL particles are oxidized once they are inside the arterial wall, aggregated, and being incorporated and taken up by macrophages and turned into foam cells. This was discussed earlier. That’s a different issue. There is no way to measure this. We just know that it is happening based on pathophysiology and autopsy results, as well as testing in animal models.
To wrap up this discussion, circulating oxidized LDL was thought to be dangerous and atherogenic. Our immune system removes oxidized particles very quickly. The amount of circulating oxidized LDL is very minimal.
Multiple articles have come out concluding that checking and relying on circulating LDL particle oxidation is inconclusive and unreliable.
References:
Micronutrient Supplementation to Reduce Cardiovascular Risk.
LOX-1 in Atherosclerosis and Myocardial Ischemia: Biology, Genetics, and Modulation.
Antioxidants and Atherosclerotic Heart Disease.
https://www.jacc.org/doi/10.1016/j.jacc.2006.03.057
https://pubmed.ncbi.nlm.nih.gov/20816951/
https://pubmed.ncbi.nlm.nih.gov/15467487/
https://pubmed.ncbi.nlm.nih.gov/18091649/
Still Have Questions? Stop Googling and Ask Dr. Alo.
You’ve read the science, but applying it to your own life can be confusing. I created the Dr. Alo VIP Private Community to be a sanctuary away from social media noise.
Inside, you get:
-
Direct Access: I answer member questions personally 24/7/365.
-
Weekly Live Streams: Deep dives into your specific health challenges.
-
Vetted Science: No fads, just evidence-based cardiology and weight loss.
Don't leave your heart health to chance. Get the guidance you deserve. All this for less than 0.01% the cost of health insurance! You can cancel at anytime!
[👉 Join the Dr. Alo VIP Community Today]