Is Salt Burning Your Heart? The Truth About Sodium & Hypertension
Dec 29, 2025
Salt, Hypertension, and Heart Disease: A Cardiologist’s Warning
I am asked about salt intake every day on social media. there is a large campaign by social media healthfluencers and medfluencers to downplay the danger of salt intake. Salt can increase inflammation as well as many factors that play a direct role in heart disease.
High sodium intake increases cardiovascular disease risk and mortality in a dose-dependent manner, while moderate sodium reduction (to <2,300 mg/day) provides cardiovascular benefits without adverse effects. The relationship is linear rather than J-shaped when sodium is measured accurately.
Doctors Diagnosing and Treating Hypertension Is Outdated
If you walk into a typical doctor's office with high blood pressure (hypertension), you usually leave with two things: a prescription for a pill and a pamphlet telling you to stop eating salt.
Six months later, you’re eating bland food, you’re miserable, and your blood pressure is still 145/90.
Why? Because for the vast majority of my patients, salt isn't the root cause. It is just the accomplice.
As a cardiologist, I view High Blood Pressure not just as a "vascular" problem, but as a metabolic problem. Here is the truth about the "Silent Killer" and how to actually get your numbers down.
What is High Blood Pressure (Really)?
Think of your cardiovascular system like a garden hose.
- The Pump: Your heart.
- The Pipes: Your arteries.
- The Fluid: Your blood.
Hypertension happens when the pressure inside those pipes gets too high. Over time, this high pressure damages the inner lining of the arteries (the endothelium), leading to plaque buildup, heart attacks, strokes, and kidney failure.
We generally want your numbers below 120/80 mmHg. Once you creep over 130/80, you are in Stage 1 Hypertension.
The "Silent Killer" Trap
The most dangerous symptom of high blood pressure is nothing.
Most people have no idea they are walking around with dangerous pressures until they have a catastrophic event. You cannot "feel" it. You cannot wait for a headache or dizziness. You have to measure it.
Dr. Alo’s Pro-Tip: Are You Measuring Correctly?
Half the patients referred to me for "resistant hypertension" just have bad measuring technique!
- Feet flat on the floor (no crossed legs!).
- Back supported in a chair.
- Arm at heart level resting on a table.
- Empty bladder (a full bladder can add 10-15 points).
- Cuff size matters: If the cuff is too small for your arm, it will give a falsely high reading.
Current Evidence on Sodium and Cardiovascular Outcomes
A 2025 umbrella review of meta-analyses found that low sodium intake was associated with reduced CVD mortality (RR 0.83, 95% CI 0.73-0.95), stroke mortality (RR 0.74, 95% CI 0.57-0.95), and all-cause mortality (RR 0.88, 95% CI 0.82-0.93).[1] Each 1 g/day increase in sodium raised systolic blood pressure by 0.60 mmHg and increased CVD and stroke risks by 4% and 6%, respectively.[1]
The most rigorous evidence comes from studies using multiple 24-hour urine collections—the gold standard for sodium assessment. A 2022 New England Journal of Medicine study of 10,709 participants found that each daily increment of 1,000 mg in sodium excretion was associated with an 18% increase in cardiovascular risk (HR 1.18, 95% CI 1.08-1.29).[2] Comparing the highest to lowest quartile of sodium excretion yielded a hazard ratio of 1.60 (95% CI 1.19-2.14) for cardiovascular events.[2]
Salt J-Curve Controversy Resolved
Earlier observational studies suggested a J-shaped relationship between sodium and cardiovascular risk, but this apparent J-curve is now recognized as a methodological artifact. Studies using spot urine samples with conversion formulas to estimate 24-hour sodium excretion create spurious J-curves due to reverse causality and measurement bias. When sodium is measured accurately with multiple 24-hour urine collections, the relationship is linear.
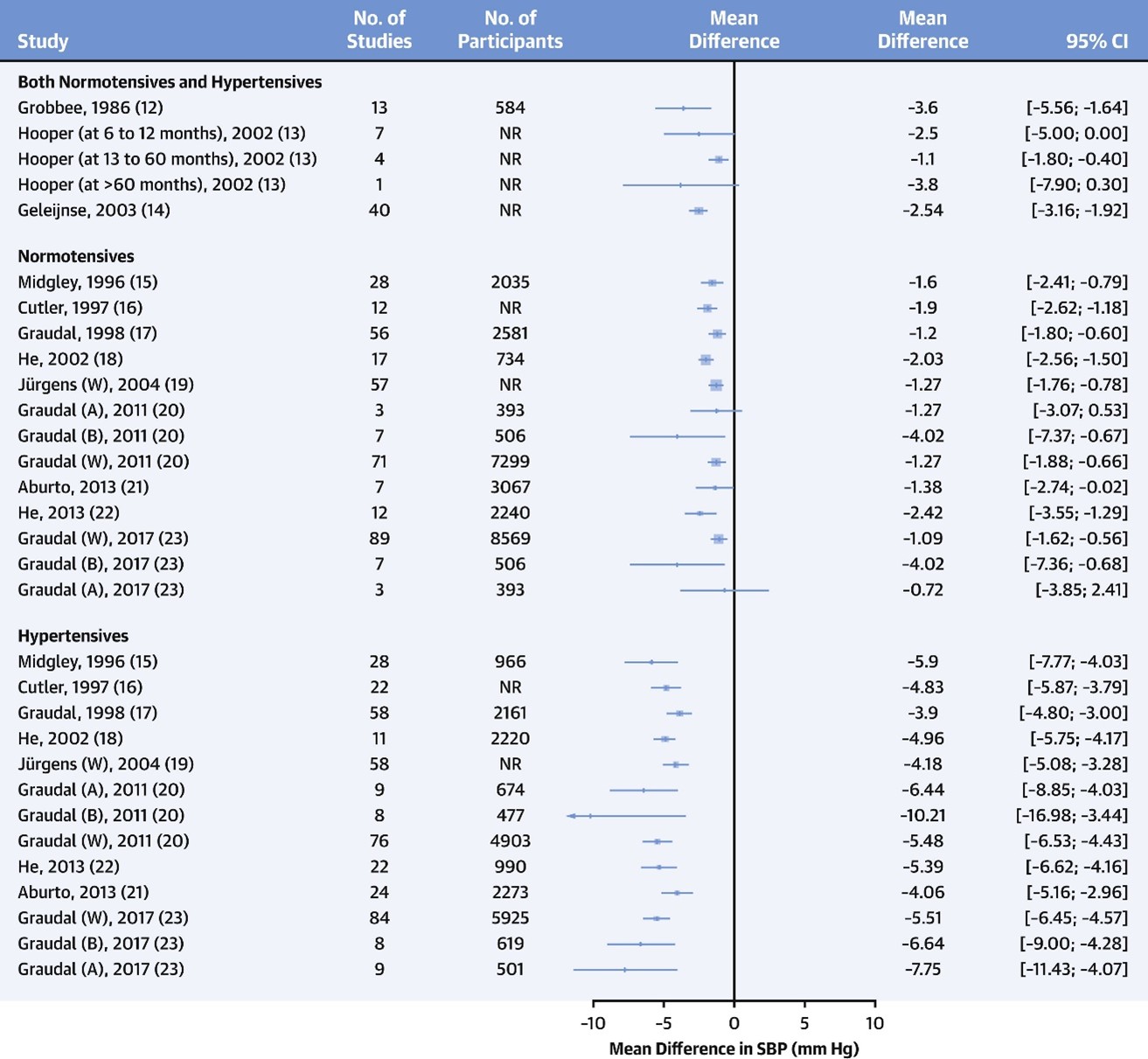
Blood Pressure Effects Of Salt
The 2025 American College of Cardiology/American Heart Association hypertension guidelines note that low-sodium (≤1,500-2,300 mg/day) versus high-sodium (≥4,500 mg/day) diets result in blood pressure reductions of approximately 3/2 mmHg in normotensive and 7/3 mmHg in hypertensive individuals. Effects are greater in Black individuals, older adults, and those with higher baseline blood pressure.
The following table from a 2017 JAMA analysis shows the relationship between sodium intake and systolic blood pressure increases across different populations:
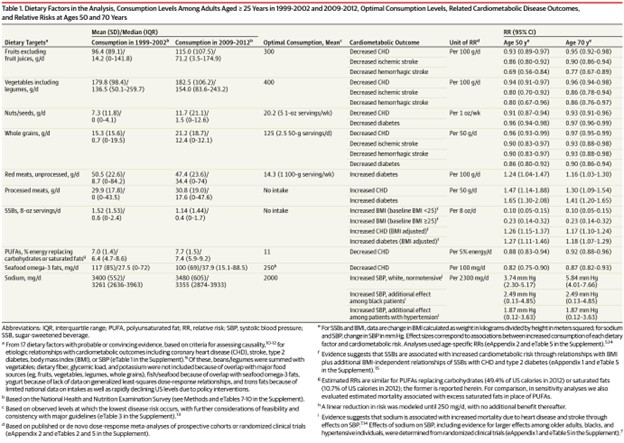
Table 1. Dietary Factors in the Analysis, Consumption Levels Among Adults Aged ≥ 25 Years in 1999-2002 and 2009-2012, Optimal Consumption Levels, Related Cardiometabolic Disease Outcomes, and Relative Risks at Ages 50 and 70 Years
Association Between Dietary Factors and Mortality From Heart Disease, Stroke, and Type 2 Diabetes in the United States. JAMA. March 6, 2017.
Population-Specific Burden Of Salt Related Heart Disease
A 2024 JAMA Network Open study of predominantly low-income Black and White Americans found that excessive sodium intake was responsible for approximately 10% of total CVD deaths and about 30% of heart failure deaths in this population. The average daily intake was 4,512 mg in Black Americans and 4,041 mg in White Americans—substantially higher than the recommended 2,300 mg/day.
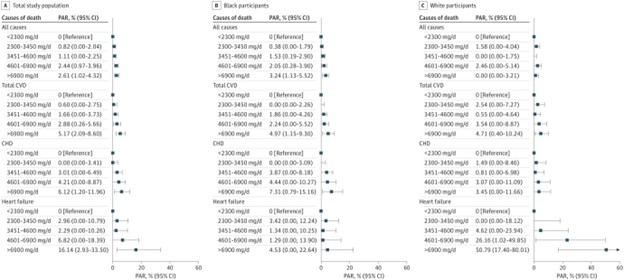
Figure 3. Population-Attributable Risk (PAR) for Cause-Specific Mortality by Dietary Sodium Intake Among Low-Income Black and White Americans
Sodium Intake and Cause-Specific Mortality Among Predominantly Low-Income Black and White US Residents. JAMA Netw Open. March 3, 2024.
Content used under license from the JAMA Network® © American Medical Association
Salt Substitutes and Interventions
The largest trial to date (SSaSS trial, n=20,995) demonstrated that salt substitutes (75% sodium chloride/25% potassium chloride) reduced systolic blood pressure by 3.3 mmHg and significantly reduced stroke, major cardiovascular events, and all-cause mortality by 12-14%.[4] Meta-analyses show no significant heterogeneity of effect by global region.
Current Salt Recommendations & Guidelines
The American Heart Association recommends choosing and preparing foods with little or no salt, targeting <2,300 mg/day for the general population.[8] The 2025 ACC/AHA hypertension guidelines emphasize that sodium reduction has additive blood pressure-lowering effects when combined with the DASH eating plan and weight loss.[4] Population-level strategies including food reformulation are essential, as most dietary sodium in the United States comes from processed foods and restaurant meals rather than salt added at the table.[4][8]
Salt As A Leading Cause Of Death
I wanted to add hypertension as its own category even though it’s not on the list of the top ten causes of death by the CDC. The burden of hypertension can be reduced by some dietary and lifestyle changes. Like what I have been discussing throughout this book, a Mediterranean style diet, just with a lot less salt, will reduce the burden of hypertension. Exercise, weight loss, quitting smoking, and reducing salt intake are the best ways to lower hypertension naturally.
Hypertension contributes to, and worsens, nearly every disease state. Just like diabetes. But hypertension is even more prevalent than diabetes.
If you read the blog on the North Karelia project, you’ll notice that they were able to reduce mortality by 84% with dietary and lifestyle changes. Forty percent of that reduction was due to reducing saturated fat intake, and 20% was due to reducing blood pressure.
Reducing salt intake can impact your blood pressure as much as taking a blood pressure medication.
Reduced salt diets, like the DASH diet, have been shown to reduce the risk of CVD.
Study:
https://www.sciencedirect.com/science/article/pii/S0735109722070371?via%3Dihub#fig1
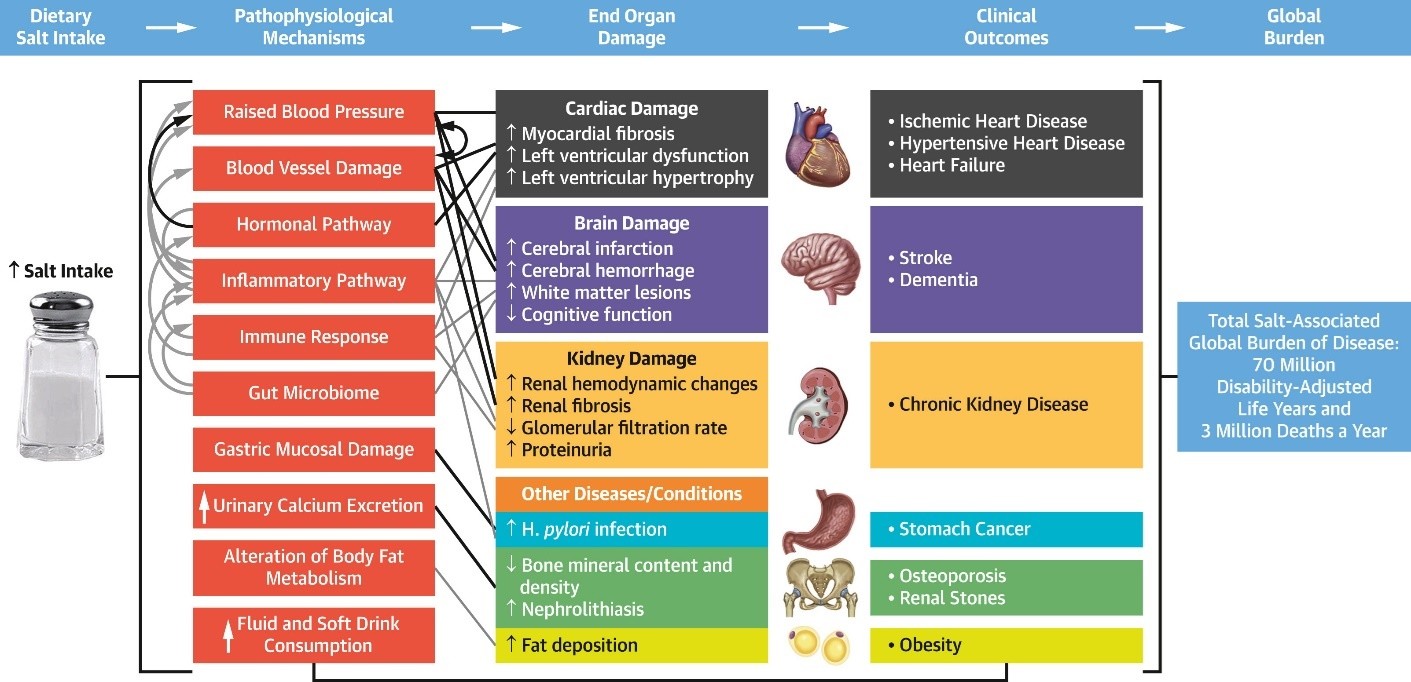
Another study published in the American Journal of Cardiology in 2020 reviewed all the available data on salt and health outcomes.
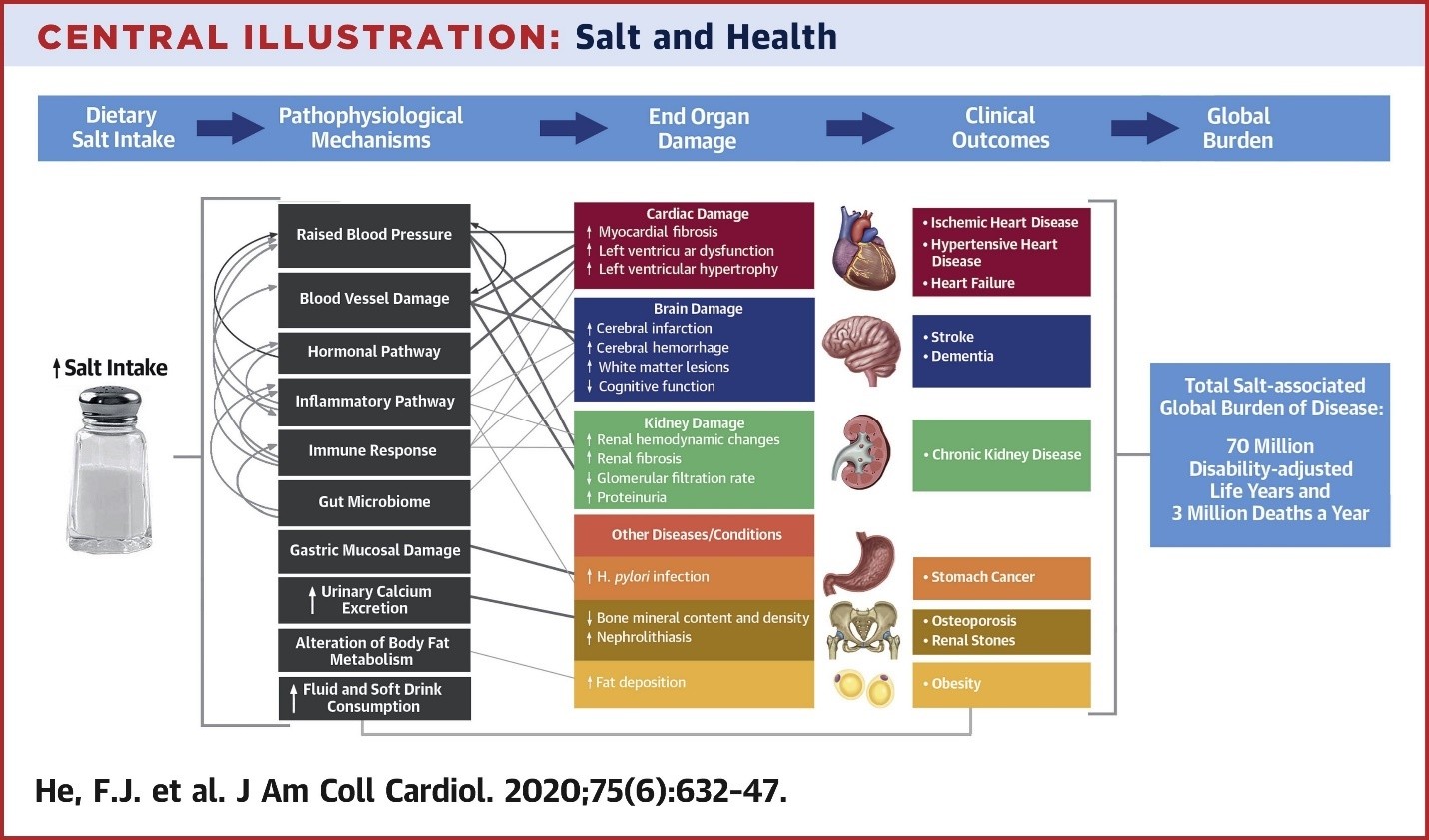
This was a meta-analysis that showed that in almost every study, reducing salt intake conferred protection and better outcomes.
From:
https://www.sciencedirect.com/science/article/pii/S0735109719386929
Salt Increases Blood Pressure & Inflammation
Every study that reduced salt intake showed a reduction in systolic blood pressure. There are a few medfluencers selling books telling you that consuming excess salt is ok.
Salt has also been shown to be highly pro-inflammatory and increases oxidative stress in humans as well as animal models. Diets that reduce salt generally reduce inflammation, blood pressure, and ASCVD.
Studies:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8399701/
https://pubmed.ncbi.nlm.nih.gov/19386745/
https://pubmed.ncbi.nlm.nih.gov/25177670/
https://pubmed.ncbi.nlm.nih.gov/16403692/
https://pubmed.ncbi.nlm.nih.gov/35883760/
https://pubmed.ncbi.nlm.nih.gov/27061200/
https://pubmed.ncbi.nlm.nih.gov/26206316/
Obviously, many people have genetically high blood pressure and there isn’t a whole lot you can do to naturally lower it. Most will need to be on medications. But you can start with a low sodium diet first and then add meds if needed.
How to Lower Blood Pressure (The Strategic Way)
If you want to get off the medication treadmill, you need a multi-pronged approach.
- Fix the Metabolism (Weight Loss)
This is the most effective "drug" we have. Losing visceral fat reduces the physical compression on your kidneys and lowers the insulin levels that cause fluid retention.
- Prioritize Sleep
Sleep Apnea is a massive cause of resistant hypertension. If you snore and have high BP, you need a sleep study. Treating apnea can sometimes cure hypertension overnight.
- Zone 2 Cardio
Low-intensity, steady-state exercise (like walking on an incline or easy cycling) helps improve the elasticity of your arteries. Flexible arteries = lower pressure.
- Don't Fear the Meds
While lifestyle is the goal, do not let your ego get in the way of safety. If your pressure is 180/100, we need to bring it down now to prevent a stroke while we work on the lifestyle changes. Medication is a bridge, not a failure.
The Bottom Line
High blood pressure is a warning light on your dashboard. You can smash the light with a hammer (take a pill and ignore the cause), or you can look under the hood.
If you are tired of generic advice and want to fix the metabolic engine driving your blood pressure, you are in the right place.
Take Control of Your Numbers
Are you confused about your meds, your diet, or your numbers? You don’t have to figure this out alone.
Inside the Dr. Alo Community, we have thousands of members reversing their metabolic numbers, sharing low-sodium (but high-flavor) recipes, and supporting each other through the journey.
[Join My VIP Community and Get Your Heart Healthy]
More References:
Annals of Medicine. 2025. Kong F, Liu Q, Zhou Q, et al.New
24-Hour Urinary Sodium and Potassium Excretion and Cardiovascular Risk.
The New England Journal of Medicine. 2022. Ma Y, He FJ, Sun Q, et al.
Salt Reduction to Prevent Hypertension: The Reasons of the Controversy.
European Heart Journal. 2021. He FJ, Campbell NRC, Woodward M, MacGregor GA.
Journal of the American College of Cardiology. 2025. Jones DW, Ferdinand KC, Taler SJ, et al. GuidelineNew
Salt Reduction to Prevent Hypertension and Cardiovascular Disease: JACC State-of-the-Art Review.
Journal of the American College of Cardiology. 2020. He FJ, Tan M, Ma Y, MacGregor GA.
The Journal of the American Medical Association. 2017. Micha R, Peñalvo JL, Cudhea F, et al.
JAMA Network Open. 2024. Yoon HS, Cai Q, Yang JJ, et al.
Circulation. 2021. Lichtenstein AH, Appel LJ, Vadiveloo M, et al.Guideline
Still Have Questions? Stop Googling and Ask Dr. Alo.
You’ve read the science, but applying it to your own life can be confusing. I created the Dr. Alo VIP Private Community to be a sanctuary away from social media noise.
Inside, you get:
-
Direct Access: I answer member questions personally 24/7/365.
-
Weekly Live Streams: Deep dives into your specific health challenges.
-
Vetted Science: No fads, just evidence-based cardiology and weight loss.
Don't leave your heart health to chance. Get the guidance you deserve. All this for less than 0.01% the cost of health insurance! You can cancel at anytime!
[👉 Join the Dr. Alo VIP Community Today]