Is HRT For Women Safe for Your Heart? Truth About MHT and Heart Disease (2026 Update)
Dec 29, 2025
Women, Menopause, Heart Disease and HRT (MHT)
Cardiovascular Disease In Women: Heart Disease is the #1 Threat to Women
Without question, heart disease is the leading cause of women in the United States and globally. As you have seen, it is very much preventable. Heart disease kills 1 in 3 women, whereas breast cancer kills 1 in 33 women. Just let that sink in.
As women go through menopause, their risk for heart disease naturally speeds up. Changes in hormones can lead to higher blood pressure, increase in LDL cholesterol, and issues with blood sugar. With over 55 million women in the U.S. currently in post-menopause, understanding the truth about Menopausal Hormone Therapy (MHT) is a major health priority. Sometimes this is called "Hormone Replacement Therapy" or HRT.
Heart disease kills more people than the top 10 cancers combined. Look at the statistics and chart and let’s dive in.

From CDC:
https://www.cdc.gov/mmwr/volumes/66/wr/mm6615a8.htm
What is Menopausal Hormone Therapy (MHT)?
Menopausal Hormone Therapy, or MHT (formerly known as HRT), is a medical treatment used to supplement the hormones—specifically estrogen and progesterone—that a woman’s body stops producing during menopause. It is primarily prescribed to provide relief from "vasomotor symptoms," which is the medical term for those disruptive hot flashes and night sweats. Depending on your health history, MHT may consist of estrogen alone (if you’ve had a hysterectomy) or a combination of estrogen and a progestogen to protect the uterine lining. While it was once thought of as a tool for heart disease prevention, we now use it as a highly effective, short-term solution for symptom management, tailored to your specific cardiovascular risk profile.
Depending on your history, MHT may be estrogen alone (if you've had a hysterectomy) or a combination of hormones.
The "Safety First" Checklist
Even though hormones are safer for younger women, they aren't for everyone. A cardiologist looks at several factors before recommending them:
Stroke and Clot Risk: Even in younger women, some forms of hormone therapy can slightly increase the risk of blood clots.
The Delivery Method: Patches and gels (transdermal) are generally safer than pills. They don't have to pass through the liver, which leads to a lower risk of clots.
Individual Risk: We must look at your blood pressure, calcium score, and pregnancy history (like having preeclampsia or gestational diabetes).
The History: Why Were We Afraid of Hormones?
For a long time, doctors prescribed hormones to help prevent heart disease. That changed in 2002 after a massive study called the Women's Health Initiative (WHI). The study was stopped early because it seemed like hormones were actually increasing the risk of heart attacks and strokes.
Because of that one study, hormone prescriptions dropped by nearly 80%. However, we now know the story is much more complex than those first headlines suggested.
The estrogen molecule plays a key role in protecting the female cardiovascular system.
Benefits of HRT MHT For Women
Women generally develop heart disease 10-15 years after their male counterparts. It was thought that estrogen was protective and offered protection up until menopausal transition (MT). MT can affect lipids adversely depending on individual genetics and other risk factors. It can affect sleep, anxiety levels, and can manifest in vasomotor symptoms.
Initially we used to give women only estrogen and it took a large clinical trial to show that CVD did not improve. Hence the guidelines have been changed and estrogen only therapy is not always recommended, but it depends on many factors.
Studies:
https://pubmed.ncbi.nlm.nih.gov/12117397/
https://pubmed.ncbi.nlm.nih.gov/15082697/
https://pubmed.ncbi.nlm.nih.gov/19468078/
Does Hormone Replacement Therapy Prevent Heart Disease?
Hormone replacement therapy (HRT) is not recommended for cardiovascular disease prevention at any age, but recent evidence supports a "timing hypothesis" suggesting that cardiovascular effects differ substantially based on when therapy is initiated relative to menopause onset.
The "Timing Hypothesis": When You Start Matters
Modern research has given us what we call the Timing Hypothesis. It turns out that the "danger" of hormones depends almost entirely on when you start them.
The Window of Opportunity: Women who start MHT before age 60, or within 10 years of their last period, often see better heart health outcomes.
The Late Starters: Women who start hormones much later (more than 20 years after menopause begins) do not see these benefits and may face higher risks.
New Findings for Younger Women
In a landmark 2025 update, researchers looked specifically at women using hormones to treat "hot flashes." The results were clear: for healthy women in their 50s, hormone therapy relieved their symptoms without raising their risk of heart disease.
In this younger age group, the actual number of "bad events" was very low—usually less than one extra case of heart trouble per 1,000 women per year.
Most Recent Updated Timing Guidelines and Hypothesis
This recent study from JAMA Internal Medicine (published in early 2025) provides a much-needed update to the Women's Health Initiative (WHI) data. It specifically looks at women who have vasomotor symptoms (hot flashes and night sweats), as these are the women most likely to seek hormone therapy in the first place.
The Main Question
Researchers wanted to know if taking Menopausal Hormone Therapy (MHT) increases the risk of heart disease specifically in women who are suffering from hot flashes and night sweats.
The Big Finding: No Increased Heart Risk
For women in their 50s (the "early menopause" group) who had moderate to severe symptoms, taking hormones did not increase the risk of:
- Heart attacks
- Strokes
- Blood clots
- Total cardiovascular disease
Relief Without the "Cost"
The study found that MHT was highly effective at relieving these symptoms. Because there was no significant increase in heart issues for this specific group, the researchers concluded that for relatively healthy women in early menopause, the benefits of symptom relief outweigh the cardiovascular risks.
Age Still Matters
The study reinforced the "Timing Hypothesis." While younger symptomatic women were safe, the data still suggests that starting hormones much later in life (age 60-70) or many years after menopause begins may carry different risks.
Why This Matters for You
This study "clears the air" for millions of women. It proves that if you are in early menopause and struggling with hot flashes, you can likely treat those symptoms with hormones without worrying that you are significantly damaging your heart health.
Source:
https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2838720
This is great news for symptomatic women. It allows us to focus on your quality of life while we continue to manage your other heart risks—like cholesterol and blood pressure—separately.
Estrogen vs. Combined Therapy: Breaking Down the Risks
Estrogen therapy (ET) was prescribed alone in women without a uterus or in those with a uterus it was combined with a progestogen (often the progestin called methyl hydroxy progesterone acetate). This is called estrogen progesterone therapy (EPT). Of note, a progestin is a synthetic progesterone- human ovaries make progesterone. The term progestogen includes progesterone and all progestins, of which, there are many.
Previously it was called HRT (hormone replacement therapy). Now it is called menopausal hormone replacement therapy or MHT. MHT includes ET and EPT.
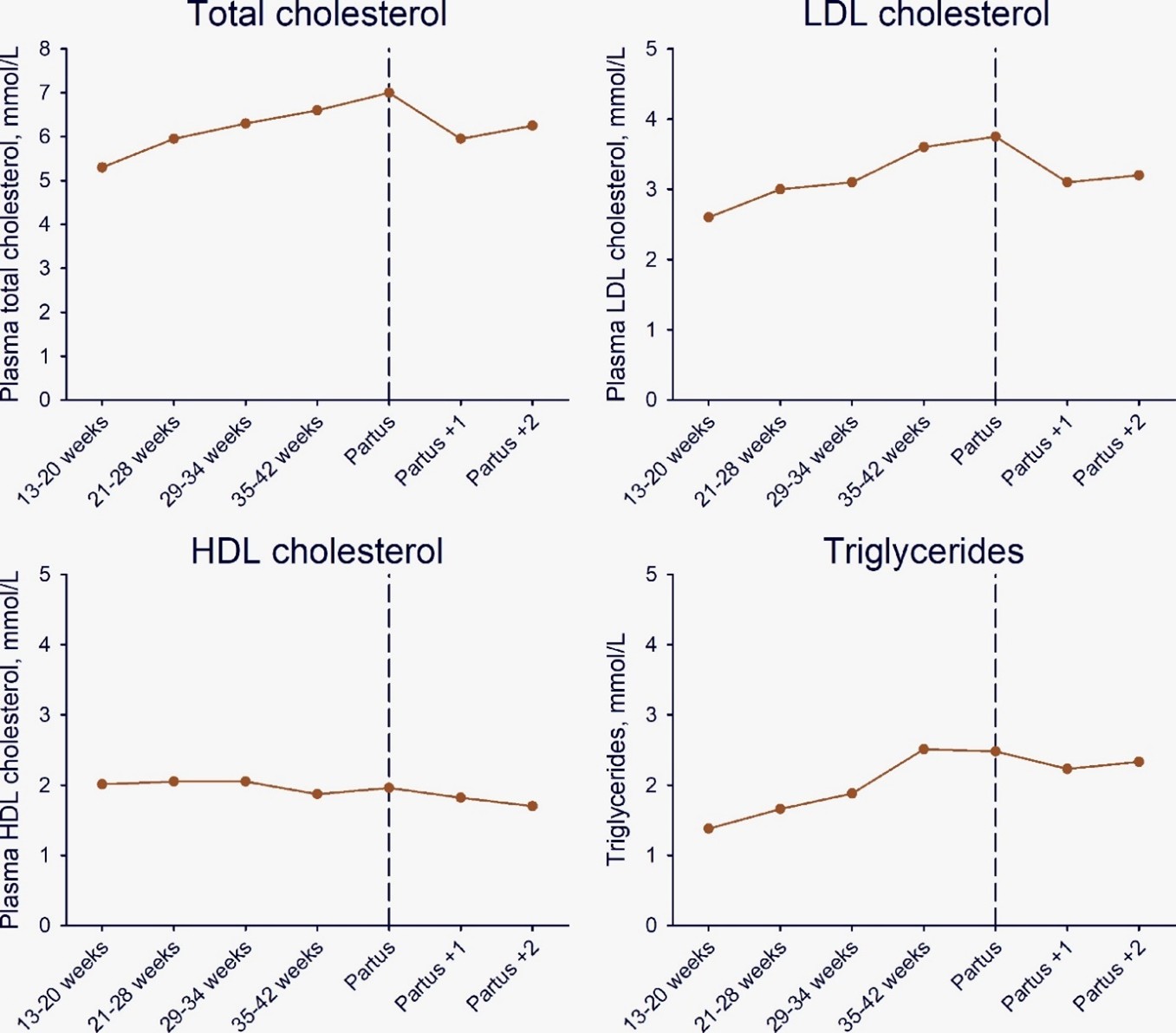
Lipids, glucose, blood pressure, obesity, vascular health, and metabolic syndrome may worsen during MT. It’s important for you and your physicians to be aware of this and adjust as necessary. Keep very good track of how you feel and what is changing. It’s not always that easy to tell.
There are approximately 55-60 million women in the United States who are pre- and peri-menopausal and need to decide on hormone replacement therapy.
There were very large databases of women established to study these effects and see if there was an effect on cardiovascular risk.
Additionally, databases were established to examine if there was a link between thromboembolic complications like pulmonary embolism (a blood clot in your lungs) or blood clots in your legs (DVT).
Does MHT Prevent Heart Disease? (The Truth)
The Women’s Health Initiative (WHI) is one of these larger studies. There are many others. The Cochrane Database is another large database to extrapolate large amounts of data and information.
In the WHI data, MHT provided no evidence for the primary or secondary prevention of all-cause mortality, cardiovascular death, nonfatal myocardial infarction, angina (chest pain) or myocardial revascularization (needing a stent or open-heart surgery to bypass blocked arteries). In fact, MHT improved all-cause mortality.
The 2015 Cochrane Database analysis comparing MHT with placebo provided risk data. MHT use was associated with an additional six strokes per 10,000 women, 8 cases of venous thromboembolism (blood clots) per 10,000 women, and four cases of pulmonary embolism (PE) per 10,000 women. This was alarming, but not an excessive amount of excess cases or risk.
Long-term mortality for MHT from the WHI disclosed no increased risk of all-cause mortality, CVD mortality or cancer mortality during 18 years of follow-up for women taking estrogen alone for a median of 7.2 years or for women taking estrogen plus medroxyprogesterone acetate for a median of 5.6 years. This was obviously very promising and helped ease fears.
Most contemporary recommendations for MHT are limited to low-risk women less than 10 years since the onset of menopause and under the age of 60 years, a different population from WHI women who were on average several years post-menopause and had worse risk factors.
The Pittsburgh WHLP (Women’s Healthy Lifestyle Project) was probably the first and probably still the only RCT (randomized control trial) designed specifically to assess the effects of a diet and exercise intervention during the MT. Can diet and lifestyle ease or improve cardiovascular risk factors in the pre and peri menopausal period?
The WHLP trial randomized 535 healthy premenopausal women 44 to 50 years of age to an assessment-only control group or a 5-year cognitive-behavioral program that included a hypocaloric diet with reduced saturated fat and cholesterol combined with moderately increased leisure-time physical activity.
An LDL-C increase in the control group during perimenopause to post menopause was blunted in the intervention group. In addition, the intervention prevented weight gain from pre menopause to perimenopause to post menopause and reduced triglycerides, systolic blood pressure, diastolic blood pressure, blood glucose, and blood insulin levels.
MHT use did not modify the associations between treatment groups and changes in LDL-C and other CHD risk factors. In addition, the intervention slowed CIMT (carotid media intimal thickening) progression among perimenopausal/postmenopausal (0.008 mm/year for the control group versus 0.004 mm/year for the intervention group), whereas no differences were seen in premenopausal women.
These were obviously all favorable and good news. The intervention group did better with lifestyle modification around the menopausal transition. Lifestyle interventions worked.
Read full WHLP article:
https://www.sciencedirect.com/science/article/pii/S0735109704009933
Persistent Risks: Stroke, VTE, and the Transdermal Advantage
Ultimately, the North American Menopause Society (NAMS), the American College of Endocrinology, and the US Preventive Services Task Force (USPSTF) also identified that MHT is neither beneficial nor indicated for preventing or reducing CVD. After reviewing all the evidence, they determined that you should not base your decision of MHT on whether or not you think it will have beneficial or negative effects on cardiovascular health.
With all of that said, many women experience severe menopausal symptoms that affect their quality of life, develop unfavorable biomarkers (insulin, lipids, fibrinogen, plasminogen, obesity, thyroid, and CRP), and report unpleasant physical effects from menopause.
MHT still remains the most effective treatment for significant vasomotor symptoms (VMS) and genitourinary syndrome of menopause. The 2017 NAMS Position Paper outlines an individual approach to CVD risk assessment and recommends low dose MHT for short periods of time for management of severe menopause symptoms. This is what most societies have adopted. Use a low dose, for as short as possible.
The American Heart Association (AHA), the American College of Cardiology (ACC) and NAMS support a customized and individualized risk assessment for women considering MHT, rather than a one size fits all, absolute recommendation. The atherosclerotic cardiovascular disease (ASCVD) pooled-cohort equation risk calculator is useful for assessing a woman's risk of CVD over the next 10 years and for her lifetime.
Calculator:
https://tools.acc.org/ascvd-risk-estimator-plus/#!/calculate/estimate/
But as I have discussed in other chapters, the 10-year risk calculators severely underestimate risk and not enough people will end up “on treatment” for elevated biomarkers and lipids. Which is why I advocate for 30-year risk assessments and very individualized care.
While many argue that the ASCVD Risk Calculator underestimates risk in women because it only includes traditional CVD risk factors and not unique risk characteristics in women, it is still probably useful for overall risk assessment and for patient education. I think for the vast majority of women, the risk calculator is good enough. But I personally prefer to be more aggressive and not wait for an event to take place.
Women And Heart Disease Risk
A recent joint Presidential Statement from the ACC and the American College of Obstetricians and Gynecologists (ACOG) recommends individual CVD risk assessment at all well-woman visits and use of the pooled-cohort equation (link above). CVD risk assessment should additionally include a history of pregnancy complications, particularly hypertension, preeclampsia and gestational diabetes, rheumatologic, and chronic inflammatory disorders in addition to traditional CVD risk factors such as smoking, high cholesterol, hypertension, diabetes, chronic kidney disease, and metabolic syndrome.
The patient’s family history and personal history should also be taken into consideration. We need to evaluate their diet, obesity, insulin resistance, advanced lipid testing, family history, smoking history, lifestyle, and many other factors. It needs to be individualized and customized.
Further, we need to evaluate whether or not they have a history of previous cancer treatment, obesity, sedentary lifestyle, high C-reactive protein, and clotting disorders should be included in the assessment for risk of VTE (venous thromboembolism) as well as for CVD.
The MHT paradox is that while hormone replacement has shown improvement in LDL-C, HDL-C, triglyceride levels and even insulin resistance, randomized controlled trials of MHT in postmenopausal women have failed to demonstrate any reduction in cardiovascular events.
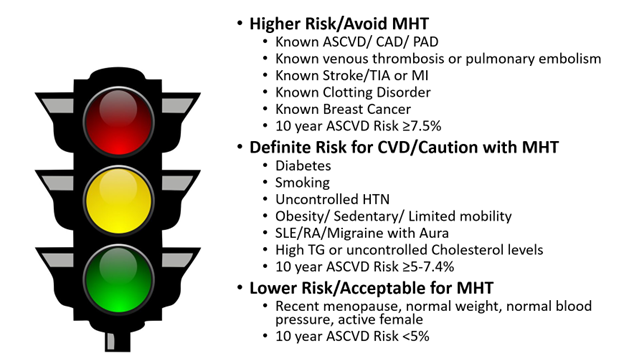
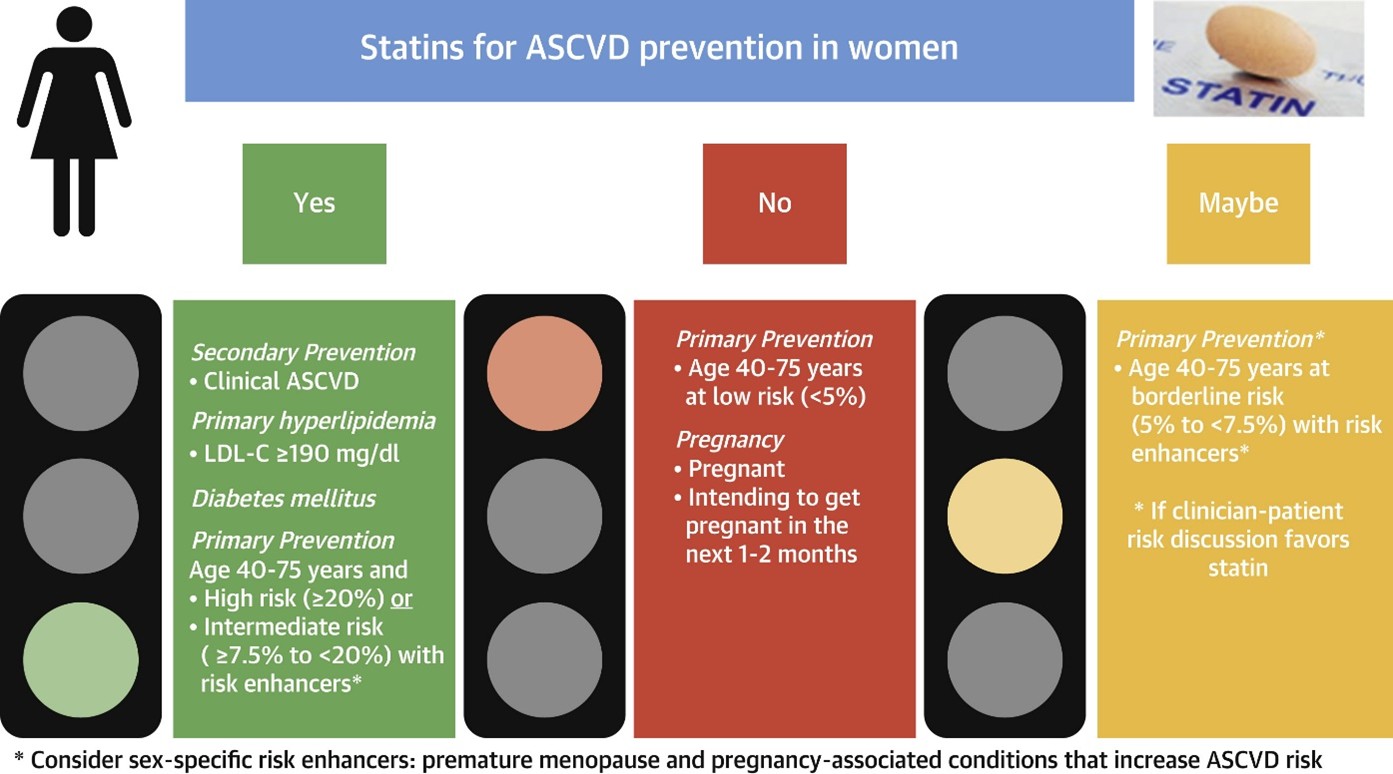
The American Heart Association and the American College of Cardiology ultimately recommend individualized decision making and being on MHT for a short period of time. They published the graphic below.
If you look at the summary graphic below, it will help you decide. If you are very high risk and have already had ASCVD or peripheral artery disease, it’s best to avoid or significantly minimize MHT/HRT and stay on lipid lowering therapy.
On the opposite end of the spectrum, if you are very low risk, quite healthy with no risk factors, you can take MHT/HRT and still try to minimize the amount of time on therapy.
If you are in between those two extremes, you need to have a serious discussion with your physician about risks versus benefits.
From:
https://www.acc.org/Latest-in-Cardiology/Articles/2019/07/17/11/56/Menopause-Hormone-Therapy
AHA Statement:
https://www.ahajournals.org/doi/10.1161/CIR.0000000000000912
Risk Calculator:
https://tools.acc.org/ascvd-risk-estimator-plus/#!/calculate/estimate/
Confusion On Women's Heart Disease Risk
Many online influencers will read the AHA statement incorrectly and think it means we should leave women alone and not treat their elevated lipid levels. This would be a huge disservice to women. They point to the statement and say that the statement itself states that there were no benefits in menopausal women for lipid lowering therapy.
This is obviously false.
Previously, cardiovascular studies didn’t include enough women, because the medical profession did not think women had heart disease. Well, they were wrong. Heart disease is the number one killer of women. They point to the study and say that, well look, women didn’t benefit from primary prevention. This is not true.
Most studies now contain equal amounts of men and women. In fact, it’s split down the middle. One thing to remember is most women don’t get heart disease until well after menopause, so short term peri menopausal studies may not show benefit. The average age of menopause in the United States is 51. Most women don’t start experiencing the symptoms of heart disease until age 65 or later. This is about a 10-15 year delay. It was previously thought that this delayed effect is due to the protective effect of estrogen, and once levels are reduced, then heart disease starts to take hold. We may not every fully understand this or have a final answer. The data has gone back and forth.
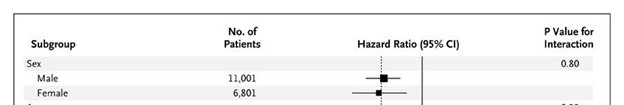
The JUPITER trial, that I have discussed extensively before, did show a 46% reduction in all endpoints for women. This was a primary prevention study of higher risk individuals with elevated hsCRP.
In the subgroup analysis in JUPITER, women benefitted more than men.

Read it again:
https://www.ahajournals.org/doi/full/10.1161/CIRCOUTCOMES.109.868299
A direct quote from the study:
“All prespecified subgroups within JUPITER significantly benefitted from rosuvastatin including those previously considered to be at “low risk” such as women, those with body mass indices less than 25 kg/m2, those without metabolic syndrome, nonsmokers, non-hypertensives, and those with Framingham Risk Scores less than 10%”.
Notice that benefits were also shown in people who were very lean and did not have metabolic syndrome. Hence, the lean mass hyper responder theory also gets thrown out the window. It doesn’t matter if you are super lean and have no insulin resistance, if you ended up with an LDL-C under 55 mg/dL, you no longer had ASCVD.
While the guidelines might not be able to say it explicitly because you need very specific and targeted data, we do know that women do benefit tremendously from lipid lowering therapy across all age groups. The JUPITER trial is just one such study that’s nearly 20 years old. We have many more.
Going even further, the European Atherosclerosis Society is recommending even more aggressive therapy for women. They note that while the heart disease is still the number one killer of women over 65 years of age, it is also the leading cause of death in middle-aged women 45-64 years of age. That cohort is growing rapidly relative to other disease states.
From study:
https://academic.oup.com/eurheartj/article/44/39/4157/7249105
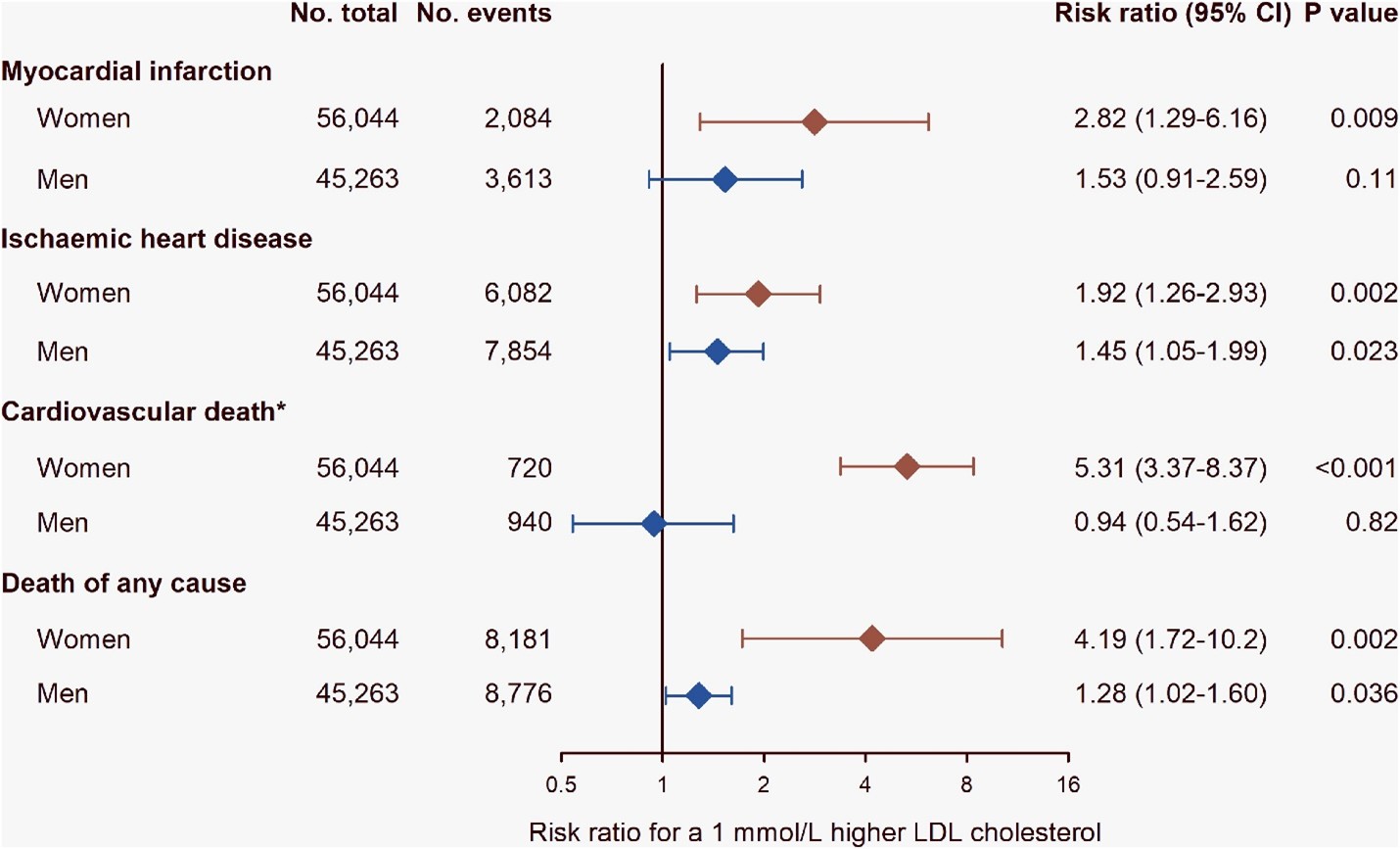
Take a look at this chart from the study. For every single measurable outcome, women had it worse for every 1 mmol/L (38.6 mg/dL) higher LDL cholesterol.
The first outcome at the top is myocardial infarction (heart attack). Women had double the risk of men for every 1 mmol/L (38.6 mg/dL) increase in LDL-C.
Look at cardiovascular death. The risk for women is 7 times that of their male counterparts.
All-cause mortality is four times higher in women than men for every 1 mmol/L increase in LDL-C.
It astonishing that we ignore our female patients and tell them that lipid lowering therapy “hasn’t been proven yet in women”. This is absurd.
Women who experience early menopause, gestational diabetes, pre-eclampsia during pregnancy, have PCOS, have auto-immune disease, have chronic kidney disease are higher risk for early ASCVD.
We also know that while men with ASCVD will first present with a cardiovascular event, women will first present with a stroke.
The European statement goes into great depth as to why estrogen and estradiol confer protection to women by reducing atherosclerotic plaque burden and nitric oxide production in the arteries. Nitric oxide helps dilate arteries to keep them open. Don’t get any ideas though, taking nitric oxide doesn’t seem to confer benefit.
Further, estrogen appears to have some anti-inflammatory effects which also help reduce the inflammatory milieu and reduce ASCVD.
Estrogen also helps to modulate reverse cholesterol transport to lower overall LDL-C levels.
Pregnancy Effects On Women And Cholesterol
All lipid levels increase with pregnancy as well.
Statin therapy is just as efficacious in men and women, as noted in many trials discussed previously.
Another very large meta-analysis looked at the Cholesterol Treatment Trialists’ Collaboration database to compare men versus women on higher versus lower intensity statin therapy. They saw a similar reduction in major coronary events, coronary revascularization, and stroke in both men and women. They also found no adverse effect on rates of cancer incidence or non-cardiovascular mortality for either sex. This translated into reductions in all-cause mortality for both men and women.
Read that study here:
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(14)61368-4/fulltext
Stop Ignoring Women's Heart Health
The EAS statement goes on to encourage the medical community to stop ignoring women and not treating them aggressively enough.
They go on to conclude, “Underappreciation of women’s ASCVD risk, missed or delayed diagnosis, and undertreatment are important contributors. Despite clear evidence that statin therapy is similarly efficacious in both sexes, women at high risk for ASCVD are less likely than men to be prescribed any statin therapy or to receive a statin at guideline-recommended intensity, and more likely to refuse or discontinue statin treatment due to perceived side effects. Clearly, action is needed to overcome these inequities”.
I highly recommend you read the full European Atherosclerosis Society statement.
Full EAS Statement:
https://academic.oup.com/eurheartj/advance-article/doi/10.1093/eurheartj/ehad472/7249105
The graphical representation of their statement is the graphic below.

You can find the above graphic at the link above from the EAS.
Back to women and risk factors.
The age at menarche (age at first monthly period) is also a risk factor. Early menarche is considered a risk factor for early ASCVD, increased risk of death from cardiovascular cause, or any cause.
This is also true for late menarche. Women who have menarche at age 17 or later are also at increased risk of cardiovascular mortality.
Parity (carrying a child and giving birth) can also affect cardiovascular outcomes. Women who have had two births have the lowest CVD risk, while women with greater than 5 births have the highest CVD risk.
Further reading.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5279938/
How Aggressively Should Women Be Treated For Heart Disease?
Should women be treated aggressively for the primary prevention of heart disease?
Should they be on statin therapy? Should they be on aspirin? Should we treat their risk factors aggressively?
It obviously depends on age and possible pregnancy.
The American College of Cardiology has published a fantastic review of the evidence. This graphic is from that review. Link to the summary is below the graphic.
Read the Summary of the Updated Guidelines for the Primary Prevention of Cardiovascular Disease in Women in the Journal of the American College of Cardiology State of the Art Review:
https://www.sciencedirect.com/science/article/pii/S0735109720347537
My Final Thoughts on MHT/HRT
We no longer use hormone therapy specifically to prevent heart disease. However, it is a safe and effective tool for managing menopause symptoms in the right patients.
If you are under 60 and struggling with hot flashes, hormones can be a great option—as long as we are also managing your cholesterol and blood pressure. Don't let outdated headlines keep you from the relief you need.
As physicians, we should treat lipids, diabetes, blood pressure, recommend a heart healthy diet, exercise program, and refer our menopausal patients to physicians certified by the Menopause Society.
Find a Certified Menopause Practitioner:
https://www.menopause.org/
We need to do a better job and be more aggressive in treating women. We need to refer them to specialists earlier.
We have always thought of heart disease as a disease for men, but clearly, it’s also the number one cause of death among women.
References:
WHI 2024 Comprehensive Review: The Women’s Health Initiative Randomized Trials and Clinical Practice: A Review (JAMA, 2024)
This is the definitive update on the long-term findings of the WHI trials.
Vasomotor Symptoms & Heart Risk (2025 Analysis): Menopausal Hormone Therapy and Cardiovascular Diseases in Women With Vasomotor Symptoms (JAMA Internal Medicine, 2025)
A new analysis showing that MHT is neutral for heart risk in symptomatic younger women.
The "Roller-Coaster" History of MHT: Menopausal Hormone Therapy and Coronary Heart Disease: The Roller-Coaster History (Climacteric, 2024)
An excellent summary of how medical advice on hormones has evolved over the years.
USPSTF 2022 Systematic Review: Hormone Therapy for the Primary Prevention of Chronic Conditions: Updated Evidence Report (JAMA, 2022)
The report used by the U.S. Task Force to set current prevention guidelines.
Modern Risk Assessment Framework (2025): Cardiovascular Risk Associated with Menopause and MHT: A Review and Contemporary Approach (Current Atherosclerosis Reports, 2025)
Details on contemporary formulations like transdermal estrogen and micronized progesterone.
WHI Contributions to Heart Research (2022): Contributions of the Women's Health Initiative to Cardiovascular Research (JACC, 2022)
A deep dive into how the WHI changed our understanding of aging and heart health in women.
Still Have Questions? Stop Googling and Ask Dr. Alo.
You’ve read the science, but applying it to your own life can be confusing. I created the Dr. Alo VIP Private Community to be a sanctuary away from social media noise.
Inside, you get:
-
Direct Access: I answer member questions personally 24/7/365.
-
Weekly Live Streams: Deep dives into your specific health challenges.
-
Vetted Science: No fads, just evidence-based cardiology and weight loss.
Don't leave your heart health to chance. Get the guidance you deserve. All this for less than 0.01% the cost of health insurance! You can cancel at anytime!
[👉 Join the Dr. Alo VIP Community Today]