Do Statins Work In Women? Benefits And Side Effects
Dec 30, 2025
How Statins Help Prevent Heart Disease in Women: A Simple Guide
What Are Statins and What Do They Do?
Statins are cholesterol-lowering medications that help prevent heart attacks, strokes, and death from heart disease in women just as well as they do in men. Think of cholesterol like grease building up in your kitchen pipes—over time, it can clog the pipes and cause problems. Statins help keep your blood vessels clean by lowering the "bad" cholesterol (called LDL cholesterol) in your blood.
How Well Do Statins Work in Women?
Large studies involving over 40,000 women have shown that statins reduce heart attacks, strokes, and death from heart disease by about 13-20% in women, which is the same benefit men get from taking these medications.
Here's what that means in real numbers: If 1,000 women at risk for heart disease take a statin for one year, the medication will prevent about 1-2 deaths and 12 major heart problems like heart attacks or strokes. The benefit gets even bigger the longer you take the medication and the higher your risk is to begin with.
Who Should Consider Taking a Statin?
Doctors recommend statins for women in several situations:
- Women who already have heart disease (like those who've had a heart attack or stroke before)
- Women with very high cholesterol (LDL cholesterol ≥190 mg/dL)
- Women with diabetes who are between 40-75 years old
- Women aged 40-75 who have risk factors for heart disease (like high blood pressure, high cholesterol, diabetes, or smoking) and whose calculated 10-year risk of having a heart attack or stroke is 10% or higher
Special Considerations for Women
Doctors now recognize that certain conditions unique to women can increase heart disease risk. These include:
- Early menopause (before age 40)
- Pregnancy complications like preeclampsia or gestational diabetes
- Polycystic ovary syndrome (PCOS)
When women have these conditions, doctors may recommend starting a statin even if their cholesterol isn't extremely high, because these factors increase their overall risk.
An Important Gap: Women Aren't Getting Statins as Often as They Should
Even though statins work just as well in women as in men, studies show that women are less likely to be prescribed statins and less likely to take them consistently. This is a problem because it means many women aren't getting the protection they need from heart disease.
Some reasons for this gap include:
- Women are more likely to decline taking a statin when it's first offered
- Women are less likely to continue taking their statin medication over time
- Doctors sometimes don't prescribe statins to women as often as they should
What About Side Effects?
The most common side effect of statins is muscle aches or pain. Women may be slightly more likely to experience muscle symptoms from statins than men, though large studies haven't found major differences in side effects between the sexes.
If you experience muscle pain while taking a statin, don't just stop taking it—talk to your doctor. There are several solutions:
- Trying a different type of statin
- Taking a lower dose
- Taking the statin less frequently (like every other day)
- Switching between different statin medications
Important Warning for Women Who Might Get Pregnant
Statins should not be taken during pregnancy. If you're a woman of childbearing age who's sexually active and taking a statin, you should use reliable birth control. If you're planning to get pregnant, stop taking the statin 1-2 months before trying to conceive. If you accidentally get pregnant while taking a statin, stop the medication immediately and call your doctor.
The only time we may make an exception for this is for women with familial hypercholesterolemia and incredibly high LDL-C. This would only be in the last trimester and would be rosuvastatin 5 mg daily. This would be under supervision of a cardiologist or a lipidologist.
Benefits of Statin Therapy in Women for Cardiovascular Disease Prevention
Statin therapy reduces cardiovascular events and all-cause mortality in women to a similar degree as in men, with the benefit clearly established for both primary and secondary prevention, though women remain less likely to receive guideline-recommended statin therapy.
Equivalent Benefit Between Sexes
Two large meta-analyses including over 40,000 women have demonstrated similar cardiovascular benefits of statin therapy in women and men for both primary and secondary prevention, with benefits seen across all levels of risk. The landmark Cholesterol Treatment Trialists' Collaboration meta-analysis of 27 randomized controlled trials involving 174,000 patients found that statins had similar effectiveness for prevention of ischemic events among men and women.
For secondary prevention specifically, a sex-based meta-analysis found that statin therapy significantly reduced any cardiovascular event with nearly identical effect sizes: women showed a pooled relative risk of 0.81 while men demonstrated a relative risk of 0.82, both highly significant with no statistical interaction between sex and treatment effect.
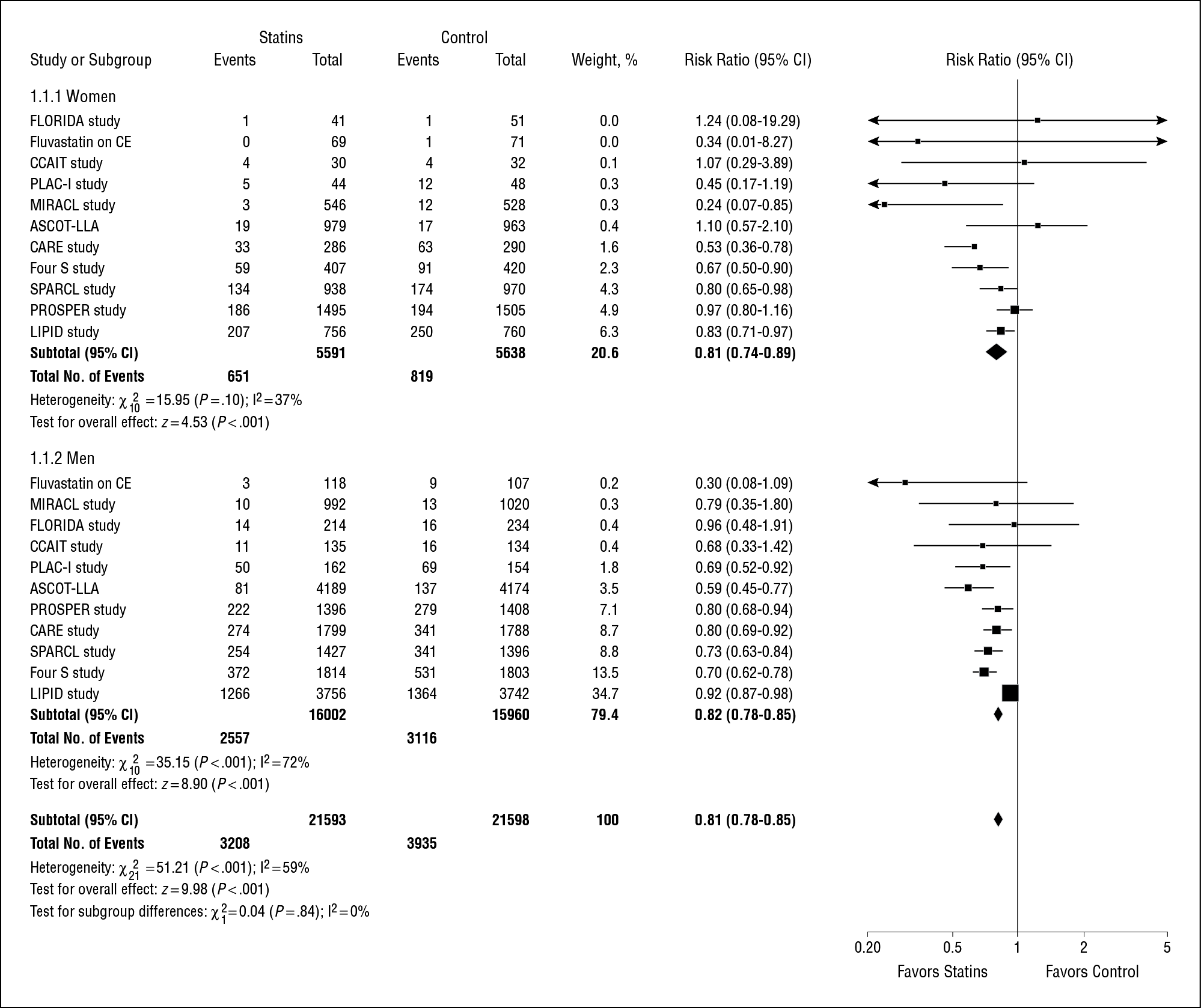
Figure 2.
Statin Therapy in the Prevention of Recurrent Cardiovascular Events: A Sex-Based Meta-analysis. Arch Intern Med. June 24, 2012.
Statin Primary Prevention Benefits In Women
In primary prevention, statins reduce major cardiovascular events by approximately 26% and all-cause mortality by 20% in the general population over one year, with greater absolute benefits in patients at higher baseline risk. The JUPITER trial, which included 6,801 women with LDL-C <130 mg/dL and elevated high-sensitivity C-reactive protein, demonstrated consistent benefit across diverse populations including substantial representation of women.
However, some meta-analyses analyzing primary prevention trials separately in women have shown mixed results. While simultaneous incorporation of both primary and secondary prevention trials strengthened the finding of CVD reduction in women, when analyzed separately, some studies showed significant reduction in coronary heart disease events in secondary prevention (RR 0.80) but not in primary prevention (RR 0.87).
Current Guideline Recommendations
There are currently no sex-specific guidelines for statin therapy, and statins should be considered at recommended doses in women who meet criteria for guideline-recommended patient populations.[1] The 2018 ACC/AHA guidelines recommend statin therapy in four groups:
- Clinical atherosclerotic cardiovascular disease
- Severe hypercholesterolemia (LDL-C ≥190 mg/dL)
- Diabetes mellitus in adults aged 40-75 years
- Primary prevention in adults aged 40-75 years at high risk (≥20%) or intermediate risk (≥7.5% to <20%) with risk enhancers
The U.S. Preventive Services Task Force recommends statin therapy for adults aged 40-75 years with one or more CVD risk factors and an estimated 10-year CVD risk of 10% or greater (Grade B recommendation), with selective offering for those with 7.5% to <10% risk (Grade C recommendation).
I normally recommend that all individuals LDL-C be below 100 mg/dL. If you have one risk factor, then under 70 mg/dL. If you have already had a cardiovascular event, then your LDL-C needs to be under 55 mg/dL. If you have gad multiple cardiovascular events, are very high risk, or have elevated lipoprotein a, your LDL-C needs to be under 40 mg/dL.
Female-Specific Risk Enhancers
The 2018 ACC/AHA guidelines include sex-specific risk-enhancing factors to help identify women at increased cardiovascular risk, including premature menopause (age <40 years) and history of pregnancy-related conditions such as preeclampsia. These risk enhancers can inform decisions about statin initiation in women with borderline or intermediate risk.
Treatment Gaps and Disparities
Despite equivalent benefit, women are less likely to receive guideline-recommended statin therapy compared with men, more likely to decline initial treatment, and less likely to continue prescribed therapy. Target cholesterol levels are less often achieved in women, partially reflecting lower likelihood of receiving lipid-lowering therapy prescriptions.
Safety Considerations In Women
Women of childbearing age on statin therapy who are sexually active should use reliable contraception. When pregnancy is planned, stopping statin therapy 1-2 months before attempting pregnancy is recommended. If unplanned pregnancy occurs, statins should be stopped immediately when pregnancy is discovered.
While no significant sex differences in adverse effects were identified in meta-analyses, few statin trials reported adverse drug reactions by sex. International consensus statements recognize female sex as a risk factor for statin-associated muscle symptoms.
The Bottom Line On Statins & Women
Statin therapy provides substantial cardiovascular benefit in women equivalent to that in men, reducing cardiovascular events and mortality in both primary and secondary prevention settings. The evidence supports guideline-recommended statin use in women meeting standard criteria, with consideration of female-specific risk enhancers such as pregnancy complications and premature menopause. Addressing the persistent treatment gaps—including lower prescription rates and adherence in women—represents an important opportunity to improve cardiovascular outcomes in this population.
Statins are safe and effective medications that reduce heart attacks, strokes, and death from heart disease in women by about 13-20%—the same benefit men receive. If you have risk factors for heart disease (like high cholesterol, high blood pressure, diabetes, or smoking), especially if you're between 40-75 years old, talk to your doctor about whether a statin might be right for you.
The decision to start a statin should be based on your individual risk factors, including any pregnancy-related complications you may have had, and should involve a conversation with your doctor about the benefits and potential side effects. Don't let the fact that you're a woman keep you from getting this important heart-protecting medication if you need it—the science clearly shows it works just as well for women as it does for men.
References
- Cho L, Davis M, Elgendy I, et al. Summary of Updated Recommendations for Primary Prevention of Cardiovascular Disease in Women: JACC State-of-the-Art Review. Journal of the American College of Cardiology. 2020. https://www.jacc.org/doi/10.1016/j.jacc.2020.02.068
- Gaudino M, Di Franco A, Cao D, et al. Sex-Related Outcomes of Medical, Percutaneous, and Surgical Interventions for Coronary Artery Disease: JACC Focus Seminar 3/7. Journal of the American College of Cardiology. 2022. https://www.jacc.org/doi/10.1016/j.jacc.2022.01.012
- Gutierrez J, Ramirez G, Rundek T, Sacco RL. Statin Therapy in the Prevention of Recurrent Cardiovascular Events: A Sex-Based Meta-analysis. Archives of Internal Medicine. 2012. https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/1106087
- Michael J. Arnold MD FAAFP, Jennifer Ballard-Hernandez DNP FNP-BC, Andrew Buelt DO, et al. The Management of Dyslipidemia for Cardiovascular Risk Reduction (Lipids) (2020). Department of Veterans Affairs. 2020. https://www.healthquality.va.gov/guidelines/CD/lipids/
- Ridker PM, Danielson E, Fonseca FA, et al. Rosuvastatin to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein. The New England Journal of Medicine. 2008. https://www.nejm.org/doi/full/10.1056/NEJMoa0807646
- El Khoudary SR, Aggarwal B, Beckie TM, et al. Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association. Circulation. 2020. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000912
- Shufelt CL. Statin Therapy in Midlife Women. Menopause. 2021. https://journals.lww.com/menopausejournal/Abstract/2021/04000/Statin_therapy_in_midlife_women.8.aspx
- US Preventive Services Task Force, Mangione CM, Barry MJ, et al. Statin Use for the Primary Prevention of Cardiovascular Disease in Adults: US Preventive Services Task Force Recommendation Statement. The Journal of the American Medical Association. 2022. https://jamanetwork.com/journals/jama/fullarticle/2792987
- Grundy SM, Stone NJ, Bailey AL, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2019. https://www.jacc.org/doi/10.1016/j.jacc.2018.11.003
Still Have Questions? Stop Googling and Ask Dr. Alo.
You’ve read the science, but applying it to your own life can be confusing. I created the Dr. Alo VIP Private Community to be a sanctuary away from social media noise.
Inside, you get:
-
Direct Access: I answer member questions personally 24/7/365.
-
Weekly Live Streams: Deep dives into your specific health challenges.
-
Vetted Science: No fads, just evidence-based cardiology and weight loss.
Don't leave your heart health to chance. Get the guidance you deserve. All this for less than 0.01% the cost of health insurance! You can cancel at anytime!
[👉 Join the Dr. Alo VIP Community Today]